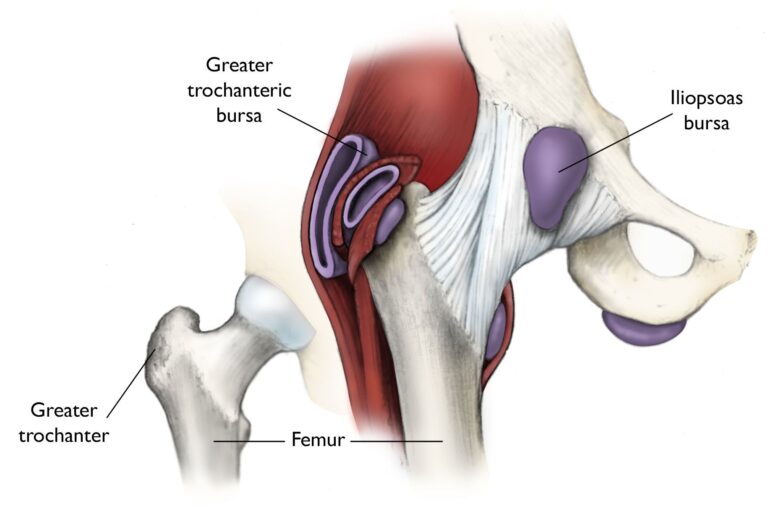
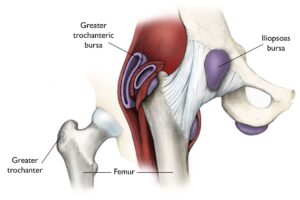
Bursae are small, fluid-filled sacs found throughout the body, including near joints such as the shoulder, elbow, hip, knee, and heel. These sac-like structures serve as cushions between bones and soft tissues, minimizing friction and promoting smooth movement.
Hip bursitis occurs when one or more of these bursae become inflamed. The hip has two main bursae that are prone to irritation and swelling. The first is the bursa overlying the greater trochanter, the prominent bony structure on the outer part of the hip. Inflammation in this area is known as trochanteric bursitis and is one of the most common forms of hip bursitis.
The second, less common type involves the iliopsoas bursa, located on the groin side of the hip. Inflammation here may also be referred to as hip bursitis, although the pain is typically concentrated in the groin. Despite the difference in location, both conditions share similar treatment approaches.
Hip bursitis most often involves the bursa that covers the greater trochanter of the femur, although the iliopsoas bursa can also become inflamed.
Your doctor will check for tenderness over the bony point of the hip bone.
Effective Nonsurgical Treatments for Hip Bursitis
For most individuals, hip bursitis can be managed effectively without the need for surgical intervention. Initial treatment typically focuses on lifestyle adjustments and targeted therapies designed to alleviate pain and inflammation. Common nonsurgical treatment options include:
- Activity Modification: Avoid activities that exacerbate symptoms, such as prolonged standing, repetitive movements, or intense physical exertion, to reduce strain on the affected hip.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Over-the-counter or prescription medications like ibuprofen, naproxen, piroxicam, or celecoxib can help manage pain and inflammation. It is crucial to use NSAIDs cautiously, especially if you have underlying medical conditions or take other medications. Consult your doctor to determine the safest option and appropriate duration for use.
- Assistive Devices: Temporary use of a walking cane or crutches can minimize pressure on the affected hip, aiding in recovery. These devices are typically recommended for a week or more, depending on the severity of symptoms.
- Physical Therapy: A physical therapy program may include exercises to stretch and strengthen the iliotibial (IT) band and hip muscles, enhancing flexibility and stability. Techniques such as rolling massage therapy, as well as the application of ice, heat, or ultrasound, may also be employed to alleviate pain and promote healing.
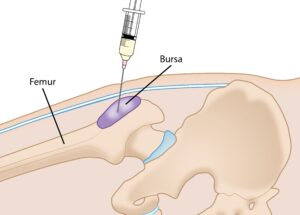
- Steroid Injections: Corticosteroid injections, often combined with a local anesthetic, can provide significant relief from pain and inflammation. This quick and minimally invasive procedure is performed in a doctor’s office and typically delivers temporary relief lasting several months. If symptoms recur, additional injections may be considered, although limiting their frequency is essential to avoid potential tissue damage. Identifying and addressing the underlying cause of bursitis remains critical for long-term management.
By following these nonsurgical approaches, many individuals experience substantial relief and improved hip function, making surgery unnecessary in most cases.