Osteonecrosis of the hip, also known as avascular necrosis (AVN) or aseptic necrosis, is a debilitating condition caused by a disruption in the blood supply to the femoral head (thighbone). Without adequate blood flow, bone cells cannot survive, leading to the gradual breakdown of the hip joint and, over time, severe arthritis.
Although avascular necrosis can affect any bone, the hip is the most commonly impacted site. Each year, over 20,000 individuals require hospitalization for treatment, with many cases involving both hips. Early diagnosis and timely intervention are essential to manage this painful condition and prevent joint degeneration.
Anatomy
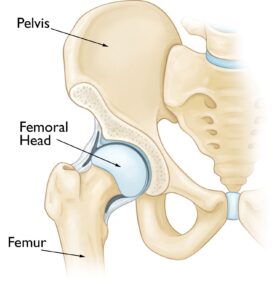
The hip joint functions as a ball-and-socket mechanism, allowing a wide range of motion.
- The socket, known as the acetabulum, is part of the pelvis.
- The ball is the femoral head, located at the upper end of the femur (thighbone).
Both the ball and socket are coated with a layer of articular cartilage, a smooth and slippery tissue that cushions the bones and facilitates seamless movement within the joint.
Causes
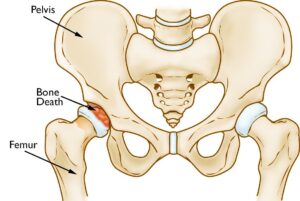
Osteonecrosis of the hip occurs when the blood supply to the femoral head is disrupted. Without sufficient blood flow, the bone tissue in the femoral head deteriorates and collapses over time. This also leads to the collapse of the articular cartilage covering the joint, resulting in severe arthritis and impaired mobility.
This condition can affect individuals of any age but is most prevalent among those aged 40 to 65. Men are more frequently diagnosed with osteonecrosis of the hip than women.
Risk Factors
While the precise cause of disrupted blood flow is not always clear, several risk factors have been linked to the development of osteonecrosis:
- Injuries: Trauma such as hip dislocations, fractures, or other injuries can damage blood vessels, restricting blood supply to the femoral head.
- Excessive alcohol consumption: Prolonged heavy drinking can lead to the formation of fatty deposits in blood vessels, reducing blood flow to bone tissue and increasing cortisone levels, which may contribute to osteonecrosis.
- Corticosteroid use: Long-term use of corticosteroid medications, often prescribed for conditions like asthma, rheumatoid arthritis, and lupus, is associated with an increased risk of osteonecrosis. While the exact mechanism is unclear, studies suggest a significant correlation.
- Underlying medical conditions: Osteonecrosis has been linked to several diseases, including:
- Caisson disease (decompression sickness or “the bends”)
- Sickle cell disease
- Myeloproliferative disorders
- Gaucher’s disease
- Systemic lupus erythematosus
- Crohn’s disease
- Arterial embolism or thrombosis
- Vasculitis

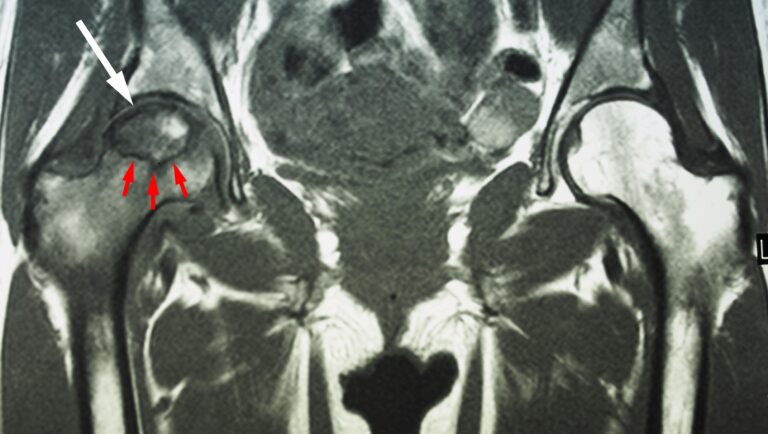


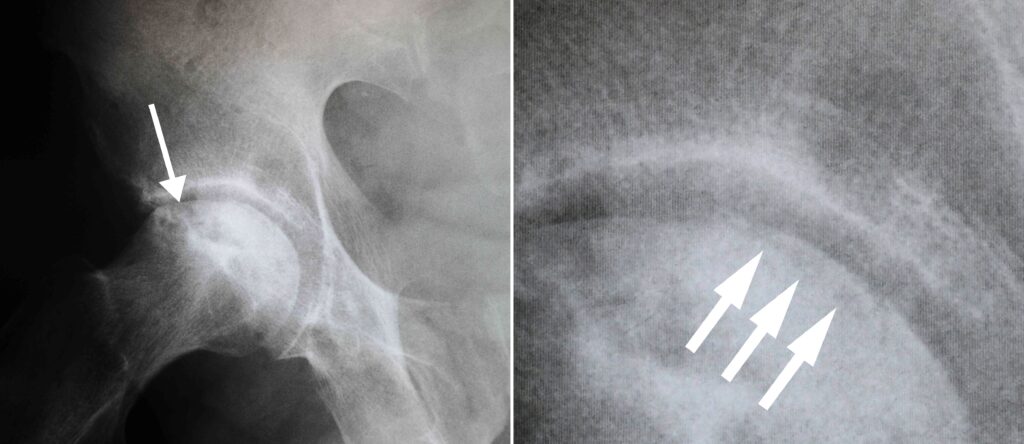
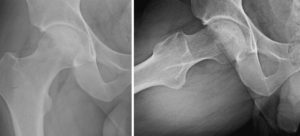
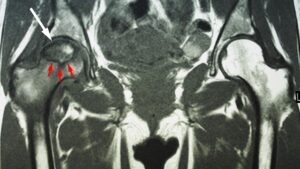 This MRI scan shows osteonecrosis in a patient’s right hip (white arrow). The dark line (red arrows) denotes the border between dead bone and living bone. The patient’s left hip is normal.
This MRI scan shows osteonecrosis in a patient’s right hip (white arrow). The dark line (red arrows) denotes the border between dead bone and living bone. The patient’s left hip is normal.