An ankle fracture, commonly referred to as a broken ankle, occurs when one or more of the bones forming the ankle joint are broken. The severity of these fractures can vary significantly, ranging from:
- Minor fractures, involving a single bone, which may allow you to continue walking with minimal discomfort, to
- Complex fractures, involving multiple bones, which often necessitate surgical intervention. Severe fractures can significantly impact mobility, preventing you from bearing weight on the affected ankle for weeks or even months. This limitation can hinder daily activities such as walking, driving, working, and participating in sports.
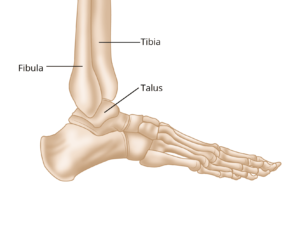
Anatomy of the Ankle: Bones and Joints Involved in Fractures
The ankle joint is composed of three key bones that work together to provide stability and movement:
- Tibia: Commonly known as the shinbone, it is the primary weight-bearing bone of the lower leg.
- Fibula: The thinner bone of the lower leg, situated alongside the tibia.
- Talus: A small bone positioned between the tibia, fibula, and the heel bone (calcaneus).
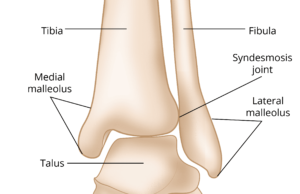
Specific parts of the tibia and fibula contribute to the ankle’s structure:
- Medial malleolus: The prominent bone located on the inner side of the ankle, at the lower end of the tibia.
- Posterior malleolus: The rear portion of the tibia.
- Lateral malleolus: The noticeable bone on the outer side of the ankle, found at the lower end of the fibula.
Ankle fractures are classified based on the location of the break. For instance:
- A fracture at the end of the fibula is referred to as a lateral malleolus fracture.
- If both the tibia and fibula are fractured, it is termed a bimalleolar fracture.
Two primary joints are involved in ankle fractures:
- Ankle Joint: The meeting point of the tibia, fibula, and talus.
- Syndesmosis Joint: The connection between the tibia and fibula, held together by strong ligaments.
Illustration showing the three bones that make up the ankle joint: the tibia, fibula, and talus.
The ankle joint allows you to bend your foot up and down and to move it from side to side. The syndesmosis joint provides stability.
Classification, Causes, and Symptoms of Ankle Fractures
Classification of Ankle Fractures
Ankle fractures are categorized based on the displacement of the broken bone fragments:
- Nondisplaced Fracture: In this type, the bones remain in their normal alignment. These fractures typically do not require surgical intervention.
- Displaced Fracture: Here, the bone fragments are separated and out of alignment. This type can involve fractures in one, two, or even three locations, often accompanied by a dislocated ankle joint. Displaced fractures, especially those with dislocations, generally require surgical treatment.
- Open Fracture: Also known as a compound fracture, this occurs when the broken bone pierces through the skin. Open fractures are considered medical emergencies due to the risk of infection from exposure to external contaminants such as dirt and debris. Immediate surgical intervention is necessary.
Causes of Ankle Fractures
Several types of injuries can result in a broken ankle, including:
- Twisting, rolling, or rotating the ankle during activities like walking or running.
- Falling from a height, such as from a ladder.
- High-impact trauma, such as that experienced in a car accident.
Symptoms of Ankle Fractures
Recognizing the symptoms of an ankle fracture is vital for prompt treatment. Common signs include:
- Severe pain that occurs immediately after the injury.
- Swelling and bruising around the ankle.
- Tenderness when the area is touched.
- Inability to bear weight on the affected foot.
- Visible deformity, particularly if the ankle joint is dislocated.
- Numbness or a cool sensation in the foot, which may indicate nerve or blood vessel involvement.
Doctor’s Examination and Treatment of Ankle Fractures
Physical Examination
To diagnose an ankle fracture, your doctor will begin by discussing your medical history and the circumstances surrounding your injury. They will then conduct a thorough physical examination of your ankle, lower leg, and foot to assess the extent of the damage.
Imaging Tests
If a fracture is suspected, your doctor may order one or more imaging tests to confirm the diagnosis and evaluate the injury:
- X-rays: These are the most common diagnostic tool for ankle fractures. X-rays provide detailed images of bones, showing the location, alignment, and number of fractured pieces. Additional X-rays of the leg and foot may be taken to check for related injuries. In some cases, a stress X-ray may be performed to assess potential damage to the syndesmosis (the joint between the tibia and fibula).
- Computed Tomography (CT) Scan: CT scans produce cross-sectional images of the ankle, offering a more detailed view of the fracture. They are especially helpful in evaluating the extent of joint involvement.
- Magnetic Resonance Imaging (MRI) Scan: MRI scans provide high-resolution images of both bones and soft tissues, such as ligaments. This imaging method is particularly useful for detecting ligament injuries that might not be visible on X-rays or CT scans.
Treatment Options
The treatment approach for an ankle fracture depends on the severity and type of injury.
Medial Malleolus Fracture
A medial malleolus fracture involves the lower portion of the tibia. These fractures can occur in isolation but are often associated with additional ankle injuries.
- Nonsurgical Treatment:
For nondisplaced fractures (where the bone remains aligned), a short leg cast or walking boot is typically used. Weight-bearing is usually avoided for several weeks, during which periodic X-rays are taken to monitor healing progress. - Surgical Treatment:
Displaced fractures (where the bone is misaligned) generally require surgical intervention. The repair may involve one or two screws to stabilize the bone. If the fracture is large or extends into the ankle joint, a combination of a plate and screws may be necessary to restore proper alignment and stability.
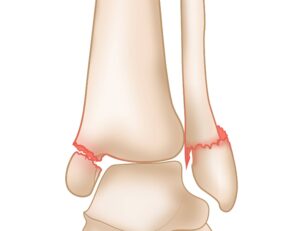
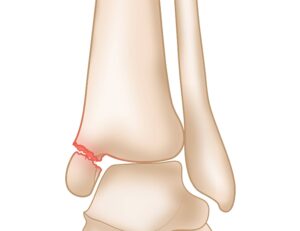 A displaced medial malleolus fracture. Note the separated bone fragments.
A displaced medial malleolus fracture. Note the separated bone fragments.
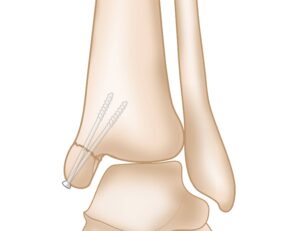 Surgical repair of displaced medial malleolus fracture with screws.
Surgical repair of displaced medial malleolus fracture with screws.
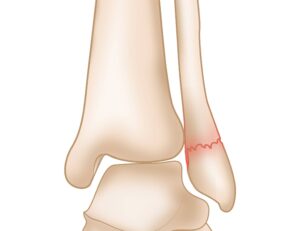
Lateral Malleolus Fracture: Diagnosis and Treatment
A lateral malleolus fracture refers to a break in the lower portion of the fibula, the smaller bone in the lower leg. These fractures are among the most common types of ankle injuries and can vary in severity.
Nonsurgical Treatment
For nondisplaced lateral malleolus fractures—where the bone fragments remain in their proper alignment—treatment typically involves the use of a short leg cast or walking boot. Unlike some other types of fractures, most isolated lateral malleolus fractures are stable enough to allow weight-bearing on the affected ankle. Your doctor will advise the appropriate level of activity and may schedule follow-up X-rays to ensure proper healing.
A lateral malleolus fracture is classified as nondisplaced when the bone fragments are not out of place.
Surgical Treatment for Lateral Malleolus Fractures
When a lateral malleolus fracture is displaced (where the bone fragments are out of alignment), surgical intervention is typically required. The procedure involves stabilizing the fracture using a combination of a plate and screws to restore proper alignment and ensure stability.
After surgery, weight-bearing on the affected ankle is generally restricted for several weeks to allow for proper healing. Your doctor will provide specific instructions for postoperative care, including follow-up appointments to monitor recovery progress and physical therapy recommendations to regain strength and mobility.
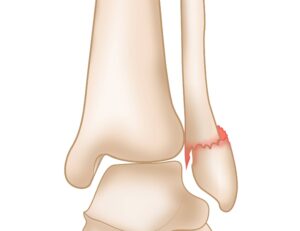 A displaced lateral malleolus fracture.
A displaced lateral malleolus fracture.
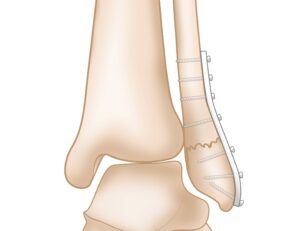
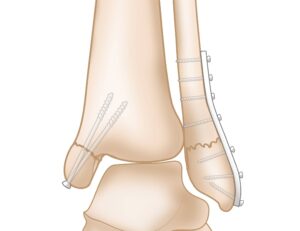
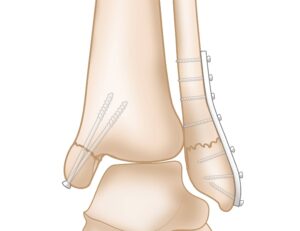
Surgical repair of displaced lateral malleolus fracture with plate and screws.
Posterior Malleolus Fracture: Causes and Treatment
A posterior malleolus fracture refers to a break in the back portion of the tibia. These fractures are often associated with other ankle injuries, most commonly a lateral malleolus fracture. This connection is due to the ligaments that link the tibia and fibula, which can transfer force between the two bones during an injury.
Nonsurgical Treatment
For small and well-aligned posterior malleolus fractures, surgery is often unnecessary. These fractures are typically treated with a short leg cast or a removable brace to immobilize the ankle and allow natural healing.
Surgical Treatment
If the fracture is large and displaced, surgical repair is required. The procedure usually involves fixing the fracture by placing screws in the lower tibia from front to back to ensure stability and proper alignment.
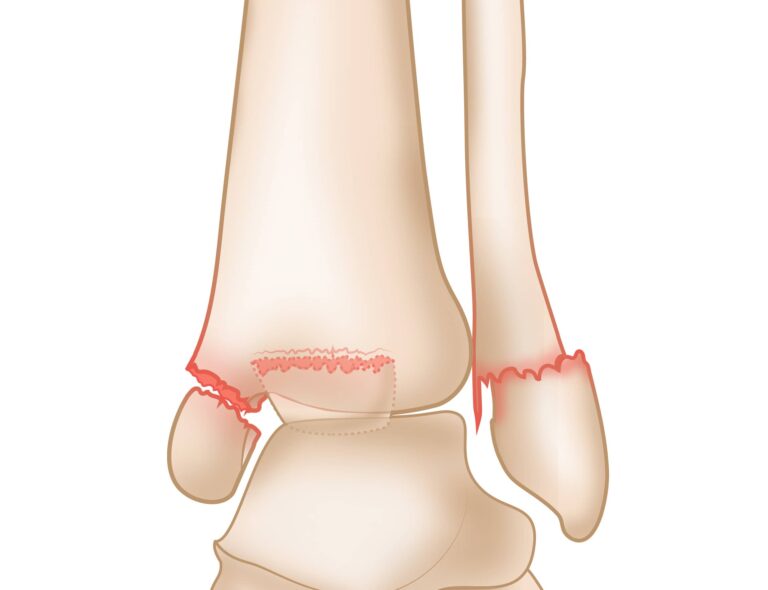
Bimalleolar and Bimalleolar Equivalent Fractures: Overview and Treatment
A bimalleolar fracture occurs when both the medial malleolus (inner side of the tibia) and the lateral malleolus (outer side of the fibula) are broken. These injuries often result in an unstable ankle, which is frequently dislocated due to damage on both sides of the joint.
Nonsurgical Treatment
In cases where the fracture is stable, a short leg cast may be used to immobilize the ankle for several weeks. During this period, patients must avoid putting weight on the injured ankle. Regular X-rays are taken to ensure the bones remain properly aligned throughout the healing process.
Surgical Treatment
Most bimalleolar fractures require surgical intervention due to the severity of the injury. The surgical procedure typically involves the use of plates and screws to stabilize both sides of the ankle and restore alignment. Proper postoperative care, including physical therapy, is crucial for regaining mobility and function.
A bimalleolar fracture occurs when both the medial malleolus (left) and lateral malleolus (right) are broken.
 Surgical repair of bimalleolar fracture with screws (medial malleolus) and plate and screws (lateral malleolus).
Surgical repair of bimalleolar fracture with screws (medial malleolus) and plate and screws (lateral malleolus).Bimalleolar Equivalent Fracture: Definition and Treatment
A bimalleolar equivalent fracture occurs when only one bone in the ankle is broken, but the ligaments on the inner (medial) side of the ankle are torn. These torn ligaments can destabilize the joint, causing the lower bone (talus) to shift out of alignment and leading to a partial dislocation or full dislocation of the ankle joint.
Treatment
Treatment for a bimalleolar equivalent fracture involves two main steps:
- Repositioning the Joint: The dislocated joint is carefully realigned to restore normal positioning.
- Repairing the Broken Bone: The fracture is stabilized, often through surgical intervention, depending on the severity of the injury and the degree of misalignment
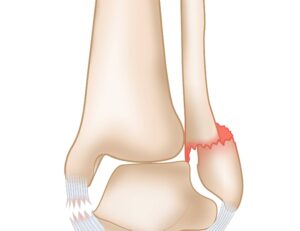 A bimalleolar equivalent fracture with torn ligaments on the medial side and a broken lateral malleolus.
A bimalleolar equivalent fracture with torn ligaments on the medial side and a broken lateral malleolus.
Trimalleolar Fracture: Understanding the Injury and Treatment
A trimalleolar fracture involves breaks in three areas of the ankle: the medial malleolus (inner tibia), lateral malleolus (outer fibula), and posterior malleolus (rear tibia). This type of injury is similar to a bimalleolar fracture but includes an additional break at the back of the tibia. Trimalleolar fractures are often unstable and can result in ankle dislocation due to the extensive damage to the joint’s structural integrity.
Treatment
- Standard Repair: In most cases, surgical repair of the medial and lateral malleolus fractures is sufficient to realign the posterior malleolus fragment, as it naturally shifts back into place during the procedure.
- Additional Surgery: If the posterior fragment remains displaced, surgical fixation is necessary. This often involves placing screws or plates to stabilize the bone and ensure proper alignment.
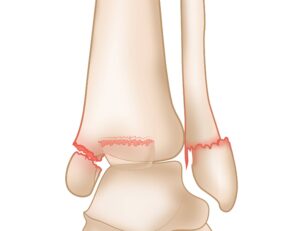 A trimalleolar fracture occurs when the medial malleolus (left), lateral malleolus (right), and posterior malleolus (middle) are broken.
A trimalleolar fracture occurs when the medial malleolus (left), lateral malleolus (right), and posterior malleolus (middle) are broken.
Syndesmosis Injury: Causes, Types, and Treatment
The syndesmosis is a group of ligaments that stabilize the small joint between the lower ends of the tibia and fibula. These ligaments play a crucial role in maintaining ankle stability during movement.
Types of Syndesmosis Injuries
- High Ankle Sprain: When the injury affects only the ligaments, it is referred to as a high ankle sprain. This type of injury can usually be treated without surgery, but recovery often takes longer compared to a typical ankle sprain.
- Syndesmosis Injury with Fracture: When the injury involves both ligament damage and one or more fractures, surgical intervention is necessary.
Treatment
- Nonsurgical Treatment: High ankle sprains, which involve only ligament sprains, are typically managed with immobilization, rest, and physical therapy. Recovery may take several weeks to months, depending on the severity.
- Surgical Treatment: When fractures are present, surgery is required to repair both the broken bone(s) and the damaged syndesmosis. The surgical procedure often involves fixing the fractures and stabilizing the syndesmosis with one or more screws. These screws may be removed later, depending on the healing progress and patient activity level.
 Surgical repair of a syndesmosis injury and lateral malleolus fracture.
Surgical repair of a syndesmosis injury and lateral malleolus fracture.
Recovery, Pain Management, and Complications After Ankle Fractures
Recovery Time
The healing time for ankle fractures varies based on the severity of the injury. While most fractures take approximately 6 weeks to heal, complete recovery—including the healing of associated ligaments and tendons—may require additional time.
Your doctor will monitor bone healing through regular X-rays during the first 6 weeks, regardless of whether you received surgical or nonsurgical treatment.
Pain Management
Pain is a natural part of the recovery process. Pain relief strategies include:
- Post-Surgery Pain Relief: Immediately after surgery, pain may be managed with intravenous (IV) medications. Once stabilized, you will switch to oral pain medications.
- Non-Surgical Pain Relief: If surgery was not required, oral medications will be used from the start.
Types of medications:
- Opioids: Effective but potentially addictive. These should be used as directed by your doctor and discontinued as your pain improves.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Help reduce pain and inflammation.
- Over-the-Counter Pain Relievers: Medications like acetaminophen may also be part of your treatment plan.
Your doctor may combine these medications to minimize the reliance on opioids.
Rehabilitation
Rehabilitation is essential to restore strength and mobility after an ankle fracture.
- Timing: Rehabilitation typically begins after the fractures have started to heal and your cast or walking boot is removed.
- Weight-Bearing: Your doctor will provide instructions on when to start putting weight on your ankle. Premature weight-bearing may disrupt the healing process.
- Physical Therapy: You may be referred to a physical therapist to develop an exercise program aimed at improving strength, flexibility, and range of motion.
You may need to wear an ankle brace during sports or other activities for several months after the fracture has healed.
Complications
Recovery from an ankle fracture may involve some complications:
- Common Issues:
- Stiffness and swelling, which may last for several months. Swelling can be managed by elevating the affected leg.
- Loss of motion, which can improve with rehabilitation.
- Healing Problems:
- Malunion: Bones heal improperly.
- Nonunion: Bones fail to heal entirely.
Surgical Complications:
- Infection
- Bleeding
- Damage to blood vessels, tendons, or nerves
- Problems with plates or screws used for stabilization
- Development of arthritis in the ankle joint
Patients with risk factors, such as smoking, diabetes, or advanced age, are more susceptible to complications after surgery.
Outcomes
Most individuals return to normal activities within 3 to 4 months of the injury. If the right ankle is affected, driving may resume after 9 to 12 weeks.
- Limping may persist for several months.
- Athletes may require extended recovery time to return to sports.
- Complete recovery from some ankle fractures, particularly severe ones, can take up to 2 years.