Understanding Posterolateral Lumbar Fusion
What Is Spinal Fusion?
Spinal fusion is a surgical procedure designed to address problems with the vertebrae (bones of the spine). The procedure acts as a “welding process,” where two or more painful vertebrae are fused together to form a single, solid bone.
The primary goal of spinal fusion is to eliminate motion between the affected vertebrae, which can often be the source of pain. By preventing movement, the fused vertebrae reduce discomfort and stabilize the spine.
Why Is Spinal Fusion Performed?
Spinal fusion is considered when pain is caused by motion between vertebrae. By stopping this movement, the pain is often significantly reduced or eliminated.
Types of Spinal Fusion
There are various techniques for spinal fusion, and your doctor will recommend the most appropriate approach for your condition. This article focuses on posterolateral lumbar fusion, the most common type of spinal fusion surgery.
What This Article Covers
This article highlights the surgical aspects of posterolateral lumbar fusion. For a comprehensive understanding of spinal fusion, including topics such as:
- Different surgical approaches
- Bone grafting options
- Potential complications
- Post-surgery rehabilitation
Consider consulting additional resources or discussing these with your healthcare provider.
Posterolateral lumbar fusion is a widely performed procedure offering significant pain relief and improved stability for patients with spinal conditions.
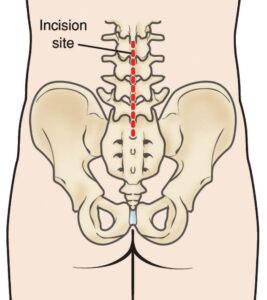
A posterior approach to lumbar surgery. An incision is made down the middle of the lower back, over the vertebrae to be fused.
Surgical Technique for Posterolateral Lumbar Fusion
Decompression Procedures
The first step of a posterolateral lumbar fusion often involves removing structures that may be putting pressure on the spinal nerves:
- Laminectomy (Decompression): The surgeon removes part or all of the lamina, the bony arch covering the spinal canal.
- Diskectomy: If a herniated or bulging disk is pressing on nerves, it is removed.
These procedures are frequently performed together to alleviate nerve compression and improve spinal function.
Bone Grafting for Fusion
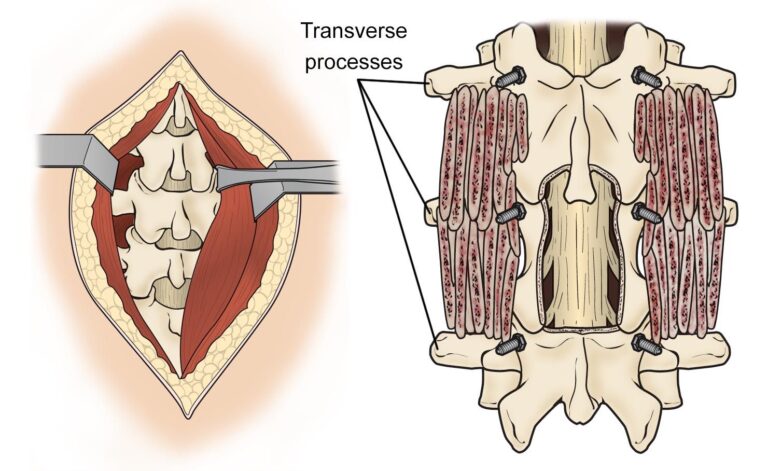
Once decompression is complete, the surgeon places bone graft material along the sides of the vertebrae to encourage new bone growth.
- Placement: The graft material is positioned over the transverse processes, which are small bony projections on either side of each vertebra.
- This technique is referred to as posterolateral fusion.
For more details on bone grafting techniques
Stabilizing the Spine
To ensure immediate stability during the healing process, titanium screws and rods are often inserted.
- These devices secure the vertebrae in place until the bone graft material achieves a solid fusion.
- Typically, the screws and rods are not removed, even after healing is complete.
This surgical technique combines decompression and stabilization to address spinal issues effectively, offering pain relief and improved function for patients.
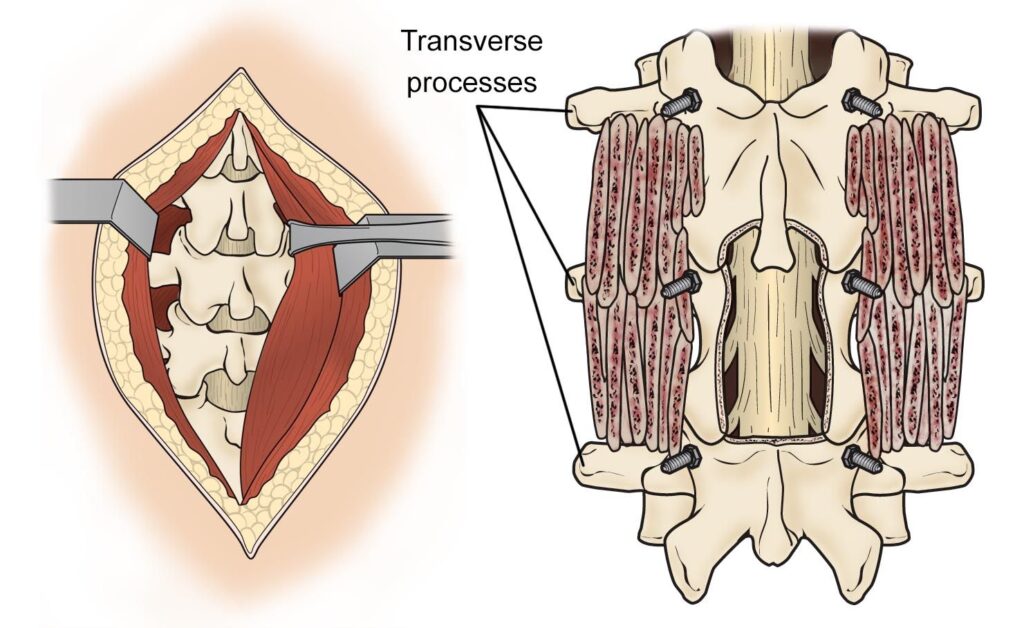
(Left) Muscles surrounding the spine are separated to expose the bone. (Right) After a decompression procedure, bone graft material is placed over the transverse processes, and screws are placed to provide stability to the spine.
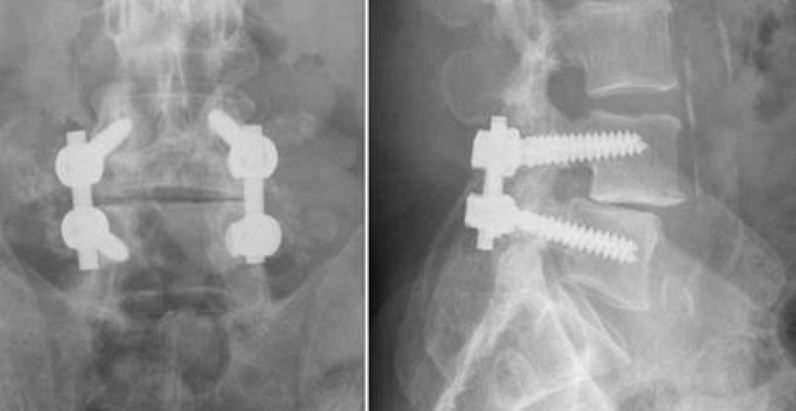
These X-rays show front and side views of posterolateral lumbar fusion.
Advantages, Disadvantages, Recovery, and Future Directions of Posterolateral Lumbar Fusion
Advantages of Posterolateral Lumbar Fusion
Posterolateral lumbar fusion offers specific benefits, including:
- Direct Nerve Relief: Provides a direct approach to alleviate pressure on spinal nerves.
- Flexibility for Revision Surgery: Allows the surgeon to remove previous hardware if necessary.
These advantages can also be achieved through other spinal fusion techniques, such as anterior (front) or lateral approaches, but the posterior route remains a versatile option.
Disadvantages of Posterolateral Lumbar Fusion
Like any surgical procedure, posterolateral lumbar fusion has potential risks:
- Nerve Damage: Can result in leg weakness.
- Hematoma: Bleeding into the muscle may compress nerves, causing weakness.
- Infection: Wound-related complications may lead to infection.
Discuss these risks with your surgeon to determine if this approach aligns with your health needs.
Recovery After Surgery
Recovery timelines and outcomes depend on the number of vertebrae fused:
- One-Level Fusion: Most patients return home the same day or the next day.
- Multiple-Level Fusion: Typically requires an overnight hospital stay.
Post-Discharge Care:
- Watch for leg weakness that causes buckling, and notify your surgeon immediately if this occurs.
- Pain medication may be needed for several days to weeks.
- A brace may be recommended to support the fusion during healing.
Outcomes of Posterolateral Lumbar Fusion
Clinical outcomes for posterolateral fusion are comparable to those of traditional spinal surgeries, providing effective pain relief and spinal stability.
Future Directions
Advancements in technology are leading to more minimally invasive techniques for posterolateral lumbar fusion. Tools like tubular retractors enable less invasive decompression and fusion, offering shorter recovery times and reduced surgical risks.
By balancing these advantages and risks, surgeons and patients can make informed decisions to optimize treatment outcomes.