Overview:
Periprosthetic glenoid fractures are rare but significant complications during shoulder arthroplasty (joint replacement surgery).
What are Periprosthetic Glenoid Fractures?
These fractures occur around the shoulder implants, either during or after shoulder arthroplasty.
Causes of Periprosthetic Glenoid Fractures:
- Patient Factors: Osteoporotic bone, delayed procedures, and bone sclerosis.
- Technical Factors: Malpositioning of implants, improper reaming techniques, and excessive force during surgery.
Symptoms:
- Pain: Severe pain around the shoulder.
- Swelling and Deformity: Visible swelling and possible deformity.
- Limited Movement: Difficulty moving the arm.
Diagnosing Periprosthetic Glenoid Fractures:
- Physical Examination: Checking for pain, swelling, and deformity.
- Imaging:
- X-rays: Standard views to assess the fracture and implant.
- CT Scans: For detailed assessment.
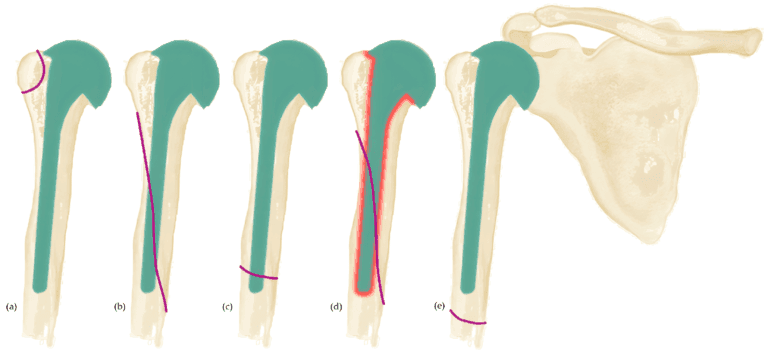
Types of Fractures:
- Type 1: Glenoid lip fractures.
- 1A: Small fractures not affecting implant stability.
- 1B: Large fractures compromising stability.
- Type 2: Scapular neck fractures affecting the glenoid and scapular body connection.
Treatment Options:
- Non-Surgical Management:
- Suitable for small, stable fractures.
- Immobilization: Using a sling or brace to support the arm.
- Surgical Management:
- Needed for larger, unstable fractures.
- Surgical Techniques: Fixation with screws, using revision components with longer pegs, and bone grafting.
Possible Complications:
- Infection: Risk after surgery.
- Implant Failure: Problems with the shoulder implant.
- Non-Union: Bone fails to heal.
Lessons Learned:
- Accurate assessment and pre-operative planning are crucial.
- Non-surgical treatment works for small, stable fractures.
- Surgery is necessary for larger, unstable fractures.
- Regular follow-up and imaging are essential for monitoring healing and detecting complications.