Introduction
Osteoporosis significantly increases the risk of compression fractures in the vertebrae, the bones forming the spine. These fractures occur when weakened bone cracks under pressure, leading to a reduction in vertebral height. In the United States alone, over 700,000 vertebral compression fractures are reported annually.
When a vertebra collapses, it can angle the spine forward, resulting in a hunchbacked posture, medically termed kyphosis. This condition often leads to chronic pain, sleep disturbances, compromised lung and digestive function, and difficulty performing daily activities.
Kyphoplasty is a minimally invasive procedure designed to restore vertebral height and strength, improving spinal alignment and alleviating pain. Studies indicate that nearly 95% of patients experience immediate pain relief following this procedure.
This guide provides essential insights into:
• The indications for kyphoplasty
• The surgical objectives and expected outcomes
• The recovery process and what patients can anticipate
Anatomy
Which Parts of the Spine Are Affected?
Each vertebra in the spine consists of a large, round structure known as the vertebral body, which provides strength and stability. Compression fractures primarily affect the front portion of the vertebral body, causing it to collapse in height while the back section remains intact. This results in a wedge-shaped deformity, leading to forward spinal angulation, a condition known as kyphosis.
Since kyphoplasty aims to restore vertebral height and structural integrity, the vertebral body is the primary focus of this procedure.
What Are the Goals of This Procedure?
Historically, open surgical techniques were employed to address osteoporotic compression fractures. However, these procedures required larger incisions, posing significant challenges due to the fragility of osteoporotic bones. Additionally, many elderly patients with fractures could not tolerate the demands of open surgery, leading to suboptimal outcomes.
Kyphoplasty offers a minimally invasive alternative, effectively stabilizing the fractured vertebra while minimizing the risks associated with open surgery, such as excessive bleeding, infection, and soft tissue trauma.
The primary objective of kyphoplasty is to restore vertebral height and stability. This is achieved by inflating a balloon inside the damaged vertebra to re-expand its structure, followed by the injection of specialized bone cement to fix the bone in place. This procedure effectively reduces pain, corrects spinal deformity (kyphosis), and enhances mobility, allowing patients to resume normal activities with minimal recovery time.
Preparations
How Should I Prepare for Kyphoplasty?
The decision to undergo kyphoplasty should be made collaboratively between the patient and the surgeon, ensuring a comprehensive understanding of the procedure. Any concerns should be discussed with the surgeon before proceeding.
Kyphoplasty is typically performed as an outpatient procedure, meaning that hospitalization is not required. Patients should avoid food and drink after midnight the night before the procedure to prepare for anesthesia.
Surgical Procedure
What Happens During the Surgery?
The patient is positioned face down on the operating table. The surgical area is cleansed with antiseptic, and a local anesthetic is administered. General anesthesia may also be used to ensure patient comfort.
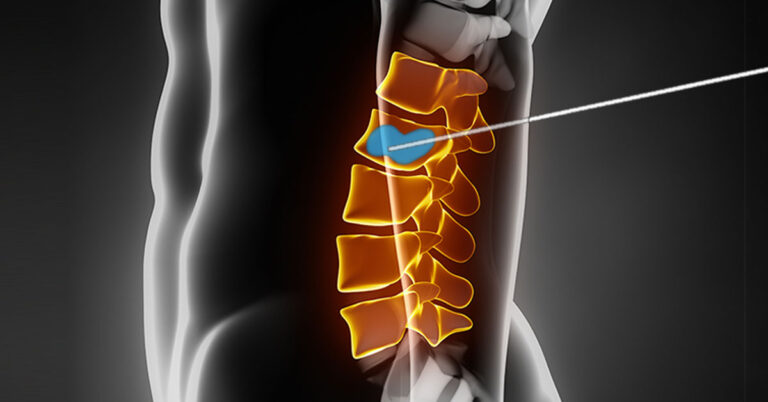
Two small incisions are made on either side of the spinal column. The surgeon inserts hollow needles into the fractured vertebra, using fluoroscopic guidance (X-ray imaging) to ensure precision. A balloon catheter is then inserted through these openings and inflated to restore vertebral height and correct kyphosis.
Once the vertebra is expanded, the balloon is removed, and bone cement is injected into the cavity. This cement hardens within 15 minutes, stabilizing the vertebra in its corrected position. The incisions are then covered with small bandages, completing the procedure.
Complications
What Are the Possible Risks?
Although kyphoplasty is considered safe and effective, complications can occur in less than 5% of cases. Potential risks include:
• Anesthesia-Related Issues – Rare reactions between anesthesia and other medications may occur. Additionally, temporary lung function impairment is possible due to anesthesia.
• Blood Clots (Thrombophlebitis) – Deep vein thrombosis (DVT) may develop postoperatively, potentially leading to a pulmonary embolism. To minimize this risk, surgeons may recommend early mobilization, compression stockings, or blood-thinning medications.
• Infection – While rare, infections can occur at the surgical site or deep within the spine, sometimes requiring antibiotic treatment or additional procedures.
• Cement Leakage – The injected bone cement occasionally escapes into surrounding tissues, though this is uncommon due to low-pressure injection techniques. In rare cases where cement presses against the spinal cord or nerves, surgical intervention may be required.
• Persistent Pain – While kyphoplasty offers significant pain relief, some patients may continue to experience mild discomfort post-procedure. Any ongoing or worsening pain should be discussed with the surgeon.
After Surgery
What Can I Expect Postoperatively?
Patients are monitored for two to three hours in the recovery unit before discharge. Some individuals may experience mild post-procedure discomfort, but hospital admission is rarely necessary.
Unlike traditional spinal procedures, kyphoplasty does not require bracing, as the hardened cement provides immediate structural reinforcement.
Rehabilitation
What Is the Expected Recovery Process?
Since the bone cement hardens within minutes, patients often experience improved mobility and reduced pain within one week. However, full recovery typically takes up to three months.
Postoperative recommendations include:
• Gradual activity resumption – Patients are encouraged to engage in light activities such as walking, avoiding strenuous exertion until medically cleared.
• Osteoporosis management – If the fracture was osteoporosis-related, the physician may prescribe calcium, vitamin D, and bone-strengthening medications to prevent future fractures.
• Lifestyle modifications – Patients are encouraged to quit smoking, engage in weight-bearing exercises, and make other bone health improvements.
For those with postural issues, muscle weakness, or persistent discomfort, physical therapy may be recommended for four to six weeks. Therapy focuses on pain relief, spinal stabilization, and posture correction to enhance long-term recovery.
As treatment progresses, patients gradually return to daily activities, often requiring only minor modifications to prevent future spinal stress.
Once rehabilitation is well established, in-person therapy sessions conclude, with patients transitioning to a long-term home exercise program.