Introduction
Arm fractures are a common occurrence in both trauma and orthopedic practice, necessitating a deep understanding of their various types, diagnosis, and treatment options. This comprehensive article is aimed at providing detailed insights into the different types of arm fractures, tailored for medical professionals. By examining classifications, treatment strategies, and complications, this article will serve as a valuable resource for doctors involved in fracture management.
1. Classification of Arm Fractures
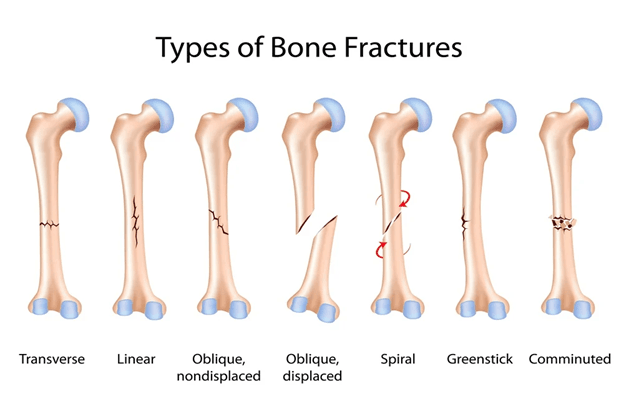
Arm fractures can be broadly classified based on the location of the fracture along the arm (proximal, midshaft, or distal), the pattern of the fracture, and whether they are open or closed. The following are the major types:
Humerus Fractures
- Proximal Humerus Fractures: Often occurring in older adults, these fractures are usually the result of low-energy falls and can be categorized further into greater tuberosity fractures, surgical neck fractures, and lesser tuberosity fractures.
- MidshaftHumerus Fractures: These fractures are common in both high-energy trauma and falls in the elderly. They can be simple, comminuted, or segmental, and the treatment may vary from conservative to surgical depending on the displacement and patient factors.
- Distal Humerus Fractures: These fractures often involve the articular surface of the elbow joint and are complex, requiring precise anatomical reconstruction to restore joint function.
Forearm Fractures
- Radius and Ulna Fractures: These can be classified into diaphyseal (midshaft), metaphyseal, and distal fractures. Fractures of the forearm bones often occur together due to their close anatomical relationship, with the Galeazzi and Monteggia fractures being classic examples.
- Galeazzi Fracture: A fracture of the distal radius with dislocation of the distal radioulnar joint.
- Monteggia Fracture: A fracture of the proximal ulna with dislocation of the radial head.
Wrist Fractures
- Distal Radius Fractures: Commonly known as Colles’ fractures, these are typically caused by falls on an outstretched hand. They can be intra-articular or extra-articular and may involve the ulnar styloid.
- Scaphoid Fractures: Due to the scaphoid bone’s poor blood supply, these fractures are notorious for delayed healing and complications such as avascular necrosis.
2. Mechanism of Injury
Understanding the mechanism of injury is crucial in diagnosing and managing arm fractures. The mechanism often determines the fracture pattern:
- High-Energy Trauma: Such as motor vehicle accidents, often results in complex fractures like comminuted or segmental fractures, which require surgical intervention.
- Low-Energy Trauma: Common in elderly patients with osteoporosis, these injuries often result in simple transverse or spiral fractures.
- Repetitive Stress: Seen in athletes, can lead to stress fractures, particularly in the midshaft of the radius or ulna.
3. Diagnosis and Imaging
Accurate diagnosis of arm fractures relies heavily on imaging. Plain radiographs are the first line of investigation, with CT scans and MRI used for more complex fractures or to assess associated soft tissue injuries. The AO/OTA fracture classification system is often used to standardize the reporting and management of fractures.
4. Treatment Approaches
Treatment of arm fractures depends on several factors including the type of fracture, patient age, bone quality, and overall health status:
- Non-Operative Treatment: Indicated for non-displaced or minimally displaced fractures. It includes immobilization with casts or braces and regular follow-up with imaging to ensure proper healing.
- Surgical Treatment: Required for displaced, open, or complex fractures. Surgical options include open reduction and internal fixation (ORIF) with plates and screws, intramedullary nailing, and external fixation. In certain cases, particularly in osteoporotic bone, joint replacement might be considered, such as hemiarthroplasty for proximal humerus fractures.
5. Complications and Management
Complications associated with arm fractures include non-union, malunion, infection (particularly in open fractures), and neurovascular injury. Understanding these complications is vital for timely intervention:
- Non-Union: May require revision surgery with bone grafting or bone stimulators.
- Malunion: Often necessitates corrective osteotomy.
- Infection: Managed with debridement and appropriate antibiotic therapy.
6. Rehabilitation and Prognosis
Rehabilitation is an integral part of fracture management. Early mobilization, guided by physiotherapy, is crucial to prevent joint stiffness and muscle atrophy. The prognosis varies based on the fracture type and the adequacy of treatment. Proximal humerus fractures, for example, may result in long-term functional impairment despite optimal treatment.
7. Frequently Asked Questions (FAQs)
Q1: What is the best imaging technique for diagnosing complex arm fractures?
- A: While plain radiographs are essential, CT scans provide detailed bone visualization, making them superior for assessing complex fractures.
Q2: How long does it typically take for an arm fracture to heal?
- A: Healing time can vary from 6 weeks for simple fractures to several months for complex or non-union cases.
Q3: What are the indications for surgical intervention in arm fractures?
- A: Surgery is indicated for displaced fractures, open fractures, fractures involving joint surfaces, and cases where conservative management fails.
Q4: Can children with arm fractures be treated differently than adults?
- A: Yes, children have a higher remodeling potential, so many fractures that would require surgery in adults can be treated conservatively in children.
Q5: What is the role of bone grafting in managing non-union fractures?
- A: Bone grafting provides the necessary osteogenic material to stimulate healing in cases of non-union, especially when biological healing potential is compromised.
Conclusion
Arm fractures encompass a broad spectrum of injuries requiring a comprehensive understanding of anatomy, biomechanics, and treatment modalities. By following the latest evidence-based guidelines and understanding the nuances of each fracture type, medical professionals can optimize outcomes for patients with these challenging injuries.
This article has been developed using insights from the Orthopaedic Trauma Association (OTA) and other leading sources in the field of orthopedic surgery.