Ankle sprains are among the most frequent injuries affecting individuals of all ages and activity levels, and they are a leading cause of missed athletic participation. These injuries occur when the sturdy ligaments stabilizing the ankle are overstretched or torn. The severity of an ankle sprain depends on the number of ligaments affected and the extent of the damage.
In most cases, ankle sprains respond well to conservative treatments, such as applying ice, elevating the ankle, using over-the-counter pain relievers, and performing basic rehabilitation exercises. However, if swelling or pain persists for several weeks, or if bearing weight on the affected ankle becomes challenging, a medical evaluation may be necessary to rule out a severe sprain or fracture.
When symptoms fail to improve with non-surgical treatments, surgical intervention might be required to repair or reconstruct the damaged ligaments. Without proper care and rehabilitation, severe or untreated ankle sprains can lead to long-term complications, such as chronic pain, arthritis, or ankle instability, increasing the risk of recurrent injuries.
Description
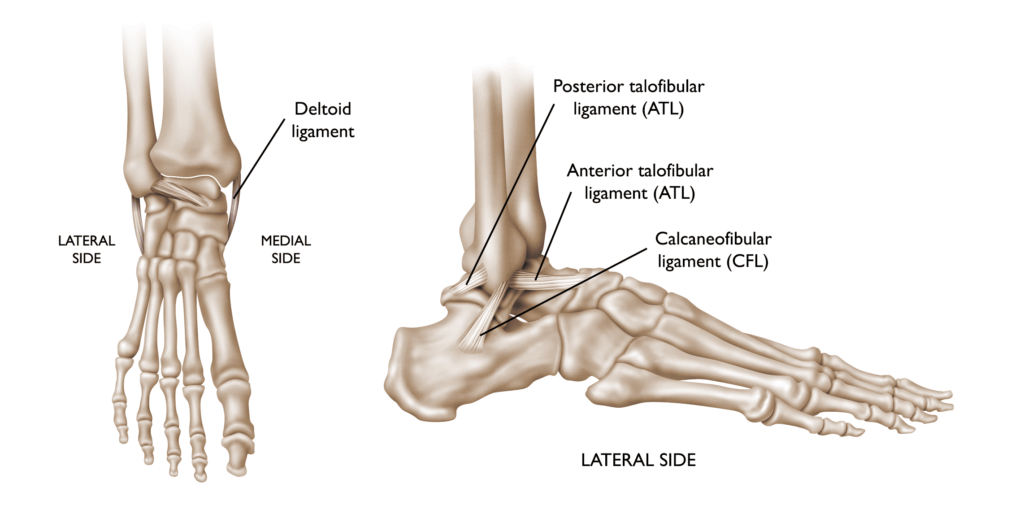
Ligaments are robust, fibrous tissues that play a vital role in connecting bones throughout the body, ensuring stability and proper alignment of joints. In the ankle, multiple ligaments work together to maintain bone positioning and provide the joint stability needed for daily activities like standing, walking, and running.
Approximately 90% of ankle sprains result from an inversion injury, where the foot turns inward, primarily affecting the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL) on the outer side of the ankle. Less commonly, medial ankle sprains occur due to eversion injuries, where the foot turns outward, damaging the deltoid ligament on the inner side of the ankle.
 An ankle sprain is an injury to one or more of the ligaments that stabilize the ankle.
An ankle sprain is an injury to one or more of the ligaments that stabilize the ankle.
The severity of a sprain can vary widely, from small tears in the ligament fibers to complete ruptures. When a ligament is completely torn, the ankle may become unstable, which can lead to progressive damage to the bones and cartilage within the joint if not properly addressed.
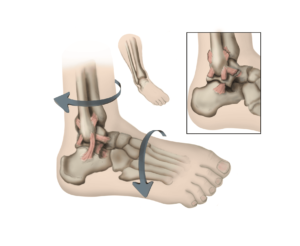 The lower leg or foot can roll, or invert, leading to a sprain of the ligaments on the outside of the ankle.
The lower leg or foot can roll, or invert, leading to a sprain of the ligaments on the outside of the ankle.
Cause
Ankle sprains frequently occur due to a sudden twisting motion of the foot or ankle. In cases of severe ligament tearing, patients may hear or feel a distinctive “pop” at the time of injury. These injuries can happen unexpectedly during various activities, including:
- Walking or exercising on uneven terrain
- Tripping or falling
- Engaging in sports that require sudden directional changes or jumping, such as basketball, tennis, soccer, football, or trail running
Symptoms
The symptoms of a sprained ankle can vary significantly depending on the severity of the injury. Common signs include:
- Pain, which may be present both at rest and during weight-bearing activities or movement
- Swelling around the affected area
- Bruising, which can range from mild to extensive
- Tenderness when the area is touched
- Ankle instability or a sensation that the ankle may give out
In severe cases, the symptoms of a sprain can closely resemble those of a fractured bone, making it essential to seek prompt medical attention to ensure an accurate diagnosis and appropriate treatment.
 Bruising and swelling are common signs of a sprained ankle. Symptom severity varies depending on the degree of injury to the ligaments.
Bruising and swelling are common signs of a sprained ankle. Symptom severity varies depending on the degree of injury to the ligaments.