CMC Joint replacement for professionals.
CMC Joint Replacement for Healthcare Professionals
Advantages of CMC Joint Replacement
- Faster Recovery Following thumb total joint arthroplasty (TJA), patients experience minimal immobilization and can resume normal activities without the need for physiotherapy. Studies show that recovery is significantly faster than after trapeziectomy. For example, data from the Swedish registry indicate that patients who undergo implant arthroplasty take an average of 94 days (men) and 109 days (women) of sick leave, compared to nearly a year for trapeziectomy patients.
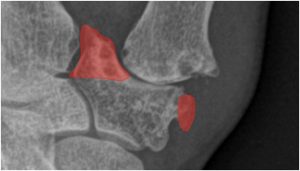
- Restoration of Thumb Length, Alignment, and Cosmesis Degenerative CMC-1 disease often causes thumb shortening and a characteristic Z-deformity due to dorsal subluxation, adduction contracture, and MCP joint hyperextension. CMC joint replacement restores thumb length and alignment more effectively than trapeziectomy. By preserving the trapezium, TJA corrects metacarpal subluxation and thumb deformities, resulting in better cosmetic outcomes and often eliminating the need for additional surgery to address MCP hyperextension.
- Prevention of Midcarpal Wrist Instability Trapeziectomy can lead to carpal instability and dorsal intercalated segment instability (DISI). Joint replacement preserves the trapezium, maintaining carpal stability and reducing the risk of postoperative dissatisfaction in patients with preoperative DISI deformity.
- Prevention of Further Degeneration of the STT Joint Removing the trapezium can result in STT joint arthritis. Total joint replacement, which preserves the trapezium, avoids this complication and extends the longevity of the surrounding joints.
- No Need to Harvest a Donor Tendon Traditional trapeziectomy often requires tendon harvesting for ligament reconstruction, which increases complications such as pain and reduced wrist strength. Joint replacement avoids tendon harvesting, offering a less invasive alternative.
- Higher Patient Satisfaction TJA patients report higher satisfaction levels (89%) compared to those undergoing trapeziectomy (76%). The faster recovery and improved function make TJA a preferable option for many patients.
- Option for Secondary Trapeziectomy In cases of prosthesis failure, patients retain the option of revision surgery or conversion to trapeziectomy. Outcomes following salvage surgery are similar to primary trapeziectomy, ensuring flexibility in future treatment options.
Disadvantages of CMC Joint Replacement
- Technically Demanding Procedure CMC joint replacement is a complex procedure requiring specialized training and experience. The learning curve is approximately 30 cases, with the risk of complications and revisions significantly reducing as surgeons gain expertise. Accurate component placement and patient selection are essential for minimizing complications.
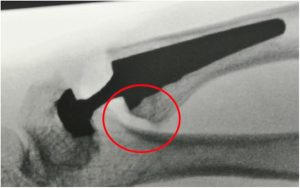
- Higher Complication Rate Complications are more frequent with TJA than with trapeziectomy, often due to technical errors. Risks include trapezium fractures, cup loosening, and implant dislocation. Proper exposure of the trapezium, fluoroscopic guidance, and careful alignment are critical for avoiding these issues.
- Increased Cost The requirement for implants increases the cost of TJA, which may deter insurance coverage despite evidence supporting its long-term benefits.
Outcome
New-generation implants with cementless fixation and a single center of rotation within the trapezium show promising durability. For instance, the ARPE prosthesis has a reported 10-year survival rate of 93%. These outcomes are comparable to hip replacements, meeting the National Institute for Health and Care Excellence (NICE) standards for joint implants.
Surgical Technique Overview
- Approach: A dorsal or lateral incision (Moberg-Gedda or Wagner approach) allows access to the CMC joint.
- Stem Placement: The volar beak of the metacarpal is resected, and the canal is prepared for the implant. Ensuring a press-fit with rotational stability, without cortical contact, reduces the risk of fractures and promotes uniform bone loading.
- Cup Placement: Correct cup positioning within the trapezium is challenging but essential for avoiding dislocation. Fluoroscopic guidance aids in accurate placement.
- Soft Tissue Management: Capsuloligamentous release of the joint is recommended to prevent ligament tethering and restricted motion.
- Correction of MCP1 Hyperextension: TJA often corrects MCP joint hyperextension automatically, though in severe cases, additional procedures such as capsulodesis may be necessary.
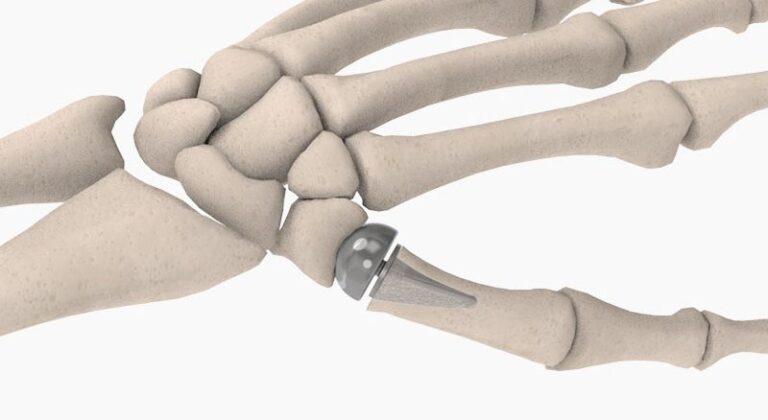
Implant System
- Cup: Titanium alloy with polar spikes for stability and hydroxyapatite coating for long-term fixation.
- Neck: Available in stainless steel or titanium (for nickel-sensitive patients), featuring a 15° offset to maintain anatomical alignment.
- Stem: Titanium alloy available in multiple sizes, designed for anatomical fit and rotational stability.
This comprehensive approach to CMC joint replacement offers significant advantages over traditional trapeziectomy, particularly in terms of faster recovery, better functional outcomes, and patient satisfaction. However, it requires technical expertise and carries a higher risk of complications, underscoring the need for careful patient selection and thorough surgical preparation.
Resection of the volar beak at the base of the thumb metacarpal.
Removal of the medial and lateral osteophytes at the distal articular surface of the trapezium.
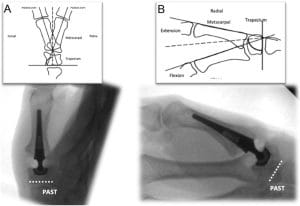
Placement of the cup in the trapezium parallel with the proximal articular surface of the trapezium aligns it with the centre of motion with the normal thumb carpometacarpal joint.
Correction of Z-deformity of the thumb by thumb carpometacarpal total joint replacement combined with volar capsulodesis of the MCP joint.
The Cup
The cup is hemispherical and composed of a titanium alloy. It features four polar spikes that provide primary stability by preventing rotation. The design also offers excellent equatorial press-fit for initial stability, with a hydroxyapatite (HA) coating to promote long-term biological fixation.
The Neck
Made of stainless steel (titanium neck available for nickel-sensitive patients) The 15˚offset neck helps to preserve the anatomical offset between the trapezium and the 1st metacarpal.
The Stem
The stem is made of titanium alloy and is available in four sizes: 7 mm (24 mm length), 8 mm (26 mm length), 9 mm (28 mm length), and 10 mm (30 mm length). It has an anatomical shape with a triangular cross-section, featuring a flat dorsal side and a curved palmar side. Scale-shaped microstructures along the edges of the stem provide primary stability, preventing both rotation and subsidence.
Exercises
Download the attached file and make sure to stick to these exercises.