Before undergoing total joint replacement surgery, your anesthesiologist — a specialist in anesthesia management — will discuss the process with you. Choosing the appropriate type of anesthesia is a critical decision that significantly impacts your recovery and comfort. This choice requires careful consideration and collaboration with both your surgeon and anesthesiologist.
Factors to Consider When Selecting Anesthesia
When deciding on the best anesthesia option, several factors should be evaluated:
- Past Experiences and Preferences:
Have you had anesthesia before? If so, were there any adverse reactions? How do family members typically respond to anesthesia? - Current Health and Physical Condition:
Are you a smoker, overweight, or undergoing treatment for other conditions alongside joint replacement? - Medication Reactions:
Do you have allergies or have you experienced side effects from certain drugs? Make sure to list all medications, supplements, and herbal remedies, especially blood thinners like Coumadin, Plavix, Eliquis, or Xarelto. - Associated Risks:
Risks vary based on your health and the type of anesthesia. They may include breathing issues, allergic reactions, or rare nerve injuries. Your medical team will thoroughly discuss potential risks with you. - Healthcare Team Expertise:
The skills and preferences of your surgical and anesthetic team play a crucial role in determining the best option.
Types of Anesthesia
Anesthesia is categorized into three main types: local, regional, and general.
1. Local Anesthesia
Local anesthesia numbs only the specific treatment area. Delivered via injection, spray, or ointment, it is typically used for minor procedures. For major surgeries, like hip or knee replacements, local anesthesia may supplement the primary anesthesia.
2. Regional Anesthesia
Regional anesthesia blocks nerves to a specific part of the body while keeping you conscious. Mild sedatives are often used to help you relax.
- Spinal Block: A short-acting anesthetic is injected into the fluid surrounding the spinal cord in your lower back. The numbing effect lasts between 1.5 to 6 hours.
- Epidural Block: A catheter delivers continuous anesthesia to the lower back for extended numbing. The catheter is placed in a slightly different spinal area than a spinal block.
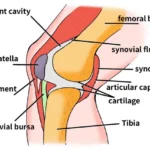
- Peripheral Nerve Block: Local anesthetic is injected around the major nerves in the thigh, such as the femoral or sciatic nerve. It numbs the targeted leg and may involve a single injection or a catheter for continuous delivery, lasting up to several days post-surgery.
Benefits of Regional Anesthesia:
- Reduced blood loss
- Decreased nausea and drowsiness
- Enhanced post-surgical pain management
- Lower risk of complications like heart attack or stroke
Possible Side Effects:
- Headaches
- Difficulty urinating
- Rare nerve injuries
- Allergic reactions
3. General Anesthesia
General anesthesia, commonly used for major surgeries, induces complete unconsciousness and acts on the brain and nervous system.
- Administration: Medications are delivered via injection or inhalation. A breathing tube is inserted to assist with oxygen supply.
- Risks and Side Effects:
- Small risks of heart attack or stroke, especially in individuals with pre-existing conditions like heart disease or COPD.
- Postoperative symptoms may include a sore throat, headache, nausea, or drowsiness.
Each type of anesthesia has unique advantages and risks. Discuss your options thoroughly with your medical team to make an informed decision that aligns with your health and surgical needs.
Pain Relief After Surgery
Effective post-operative pain management is essential for reducing discomfort, enabling movement, and facilitating participation in physical therapy after surgery.
The initial days following total hip or knee replacement surgery can be painful. To manage this, your doctor will typically prescribe a combination of oral and intravenous (IV) medications to ensure you remain as comfortable as possible.
Oral Pain Medications
Your doctor may provide a combination of oral medications to manage your pain, including:
- Non-Narcotic Pain Relievers: Medications like acetaminophen (e.g., Tylenol) can help control mild to moderate pain.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Drugs like ibuprofen or naproxen are effective in reducing inflammation and pain.
- Muscle Relaxants: Medications such as methocarbamol, cyclobenzaprine, or carisoprodol can relieve muscle tension.
- Opioid-Based Medications: Options like hydrocodone, oxycodone, or tramadol may be prescribed for managing more severe pain.
Important Note on Opioids: Use opioids only as directed by your doctor and discontinue them as soon as your pain begins to improve. While opioids are effective for short-term pain relief, they carry a risk of addiction. If your pain does not improve within a few days after surgery, consult your doctor immediately.
Intravenous Pain Medications
IV pain medications, such as morphine or hydromorphone (Dilaudid), may be used to supplement oral medications during episodes of intense pain. IV medications act quickly, providing rapid relief when pain is severe.
If your surgery involved an epidural or peripheral nerve block, the catheter may remain in place post-surgery to continue delivering anesthesia for pain control. In some cases, you may have limited control over the amount of medication administered through the catheter within preset safety limits.
Monitoring: Your medical team will closely monitor you to prevent complications such as excessive sedation or falls.
Why Proper Pain Management Matters
Appropriate use of pain medications before, during, and after surgery is crucial for promoting healing and improving your recovery experience. Proper pain control helps you:
- Move more easily.
- Actively participate in physical therapy.
- Avoid complications, such as prolonged immobility or excessive discomfort.
Take time to discuss pain relief options with your doctor before surgery. Understanding your pain management plan and asking questions will help you feel confident and prepared for your recovery.