Diabetes, a chronic condition characterized by elevated blood sugar levels, impacts approximately 9% of the U.S. population—about 30 million individuals. Among its complications, diabetic foot issues pose a significant health challenge and are a leading cause of hospitalizations.
The majority of foot complications in diabetic individuals stem from the disease’s detrimental effects on small blood vessels. In the feet, this vascular damage results in two primary problems:
- Reduced Sensation: Impaired blood flow to the nerves diminishes sensation, making individuals less aware of cuts, injuries, or trauma to their feet.
- Delayed Healing: Poor circulation to the skin and underlying tissues hinders wound healing. This increases the risk of wounds becoming chronic, providing a gateway for bacterial infections, which may lead to severe diabetic foot infections.
While numerous treatment options exist for addressing diabetic foot complications, prevention remains the cornerstone of effective management. Maintaining strict blood sugar control and conducting daily foot inspections are essential strategies for reducing the risk of these debilitating conditions.
One severe consequence of diabetic neuropathy—a type of nerve damage caused by diabetes—is Charcot arthropathy (also referred to as Charcot neuroarthropathy or Charcot foot). This condition arises from unnoticed bone injuries in the foot, potentially resulting in significant deformities and mobility issues. The following sections will delve deeper into Charcot arthropathy, its implications, and management strategies.
Description
Charcot arthropathy, also known as Charcot foot, is a severe condition of the foot and ankle caused by an inability to sense injuries. This loss of sensation can result in progressive deformities. For Charcot foot to develop, neuropathy (nerve damage) must already be present, with diabetes being the most common underlying cause.
In individuals with diabetic neuropathy, fractures or dislocations in the foot may occur without the patient being aware. These injuries can result from:
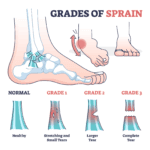
- Traumatic Events: Obvious incidents such as falls or ankle sprains.
- Chronic Microtrauma: Gradual damage due to altered weight distribution on the foot. In individuals without neuropathy, such abnormal forces typically cause pain, prompting the person to adjust their posture and redistribute weight. However, diabetic patients may not feel pain or make these adjustments, allowing repeated stress to cause fractures and other injuries over time.
Without the ability to feel pain, a person with diabetes may continue walking on an injured foot, exacerbating the damage and leading to severe deformities. Interestingly, only 25–50% of individuals with Charcot foot recall a specific injury preceding the condition.
 A severely infected big toe. This infection began two days earlier as a small blister at the tip of the toe.
A severely infected big toe. This infection began two days earlier as a small blister at the tip of the toe.
Risk Factors
While neuropathy is a prerequisite for Charcot arthropathy, other factors can increase the likelihood of its development:
- Obesity: Excess body weight places additional strain on feet with impaired sensation, significantly raising the risk.
- Age: The risk of developing Charcot foot also increases as diabetic individuals grow older.
Impact of Deformities
The deformities caused by Charcot arthropathy can lead to several complications:
- Difficulty Wearing Shoes: Severe deformities may make it impossible to find or wear normal footwear.
- Loss of Stability: Deformities can destabilize the foot and ankle, hindering the ability to walk normally.
- Increased Risk of Ulcers: The most critical concern is that deformities often result in areas where the bones protrude just beneath the skin. These pressure points can cause skin ulcers, significantly raising the risk of foot infections.
Diabetics face unique challenges in wound healing due to poor blood circulation and reduced immune response. In cases of Charcot foot, if an ulcer develops, the likelihood of amputation rises dramatically. Diabetics with Charcot foot have a 50% chance of requiring an amputation once an ulcer forms, compared to just a 10% risk without an ulcer.
 (Left) This patient with Charcot of the ankle has developed a deformity that places abnormal pressure on the outside of the ankle. (Right) This pressure has led to the development of a chronic sore (ulcer) that can be extremely difficult to treat.
(Left) This patient with Charcot of the ankle has developed a deformity that places abnormal pressure on the outside of the ankle. (Right) This pressure has led to the development of a chronic sore (ulcer) that can be extremely difficult to treat.
Symptoms
Charcot arthropathy often develops without significant pain, but patients may experience other noticeable symptoms.
- Swelling: One of the earliest signs is unexplained swelling in the foot, often without any apparent injury. Many patients first notice difficulty fitting into their usual footwear.
- Redness and Warmth: Inflammation, characterized by redness and warmth, is another early indicator. These changes occur as part of the body’s natural inflammatory response to underlying injuries in the foot.
These symptoms—swelling, redness, and warmth—can sometimes be mistaken for an infection. However, an infection is unlikely if the skin remains unbroken and no wounds are present. For a diabetic patient with a newly swollen foot and no wounds, Charcot arthropathy is the most probable diagnosis. A simple test to distinguish Charcot from an infection is to elevate the affected foot for several minutes. In Charcot, the redness, swelling, and warmth typically improve; in an infection, these symptoms usually persist.
Doctor Examination
Medical History and Physical Evaluation
During your visit, the doctor will inquire about your symptoms and overall health. Key questions may include:
- Details about any possible foot injuries.
- Information regarding your diabetes management, including your most recent hemoglobin A1C level and any history of foot wounds or infections.
Following the discussion, the doctor will conduct a thorough examination of your foot:
- Inflammation Check: If your foot is red, swollen, and warm, the doctor may elevate it to see if the symptoms subside.
- Inspection for Ulcers or Bony Prominences: They will examine the skin for any signs of ulcers or protruding bones that could cause pressure points leading to ulcers.
- Foot Shape Analysis: The doctor will assess the foot’s shape for any visible deformities and determine if these are flexible (correctible) or rigid.
- Blood Flow and Sensation Testing: Circulation and nerve function in the foot will also be evaluated.
Imaging Tests
- X-rays: X-rays are a crucial diagnostic tool for Charcot foot. In the early stages, X-rays may appear normal. However, as the condition advances, signs such as fractures, bone fragments, and joint destruction become evident. Over time, more severe deformities, dislocations, and new bone formations may develop, indicating progressive Charcot arthropathy.
 The patient shown in the X-ray had noticed swelling of the foot for approximately 3 weeks without any known injury. The X-ray shows several fractures (arrowheads) and a dislocation of the first metatarsal (arrow). Such a severe injury in patients without diabetes would be seen only after a high-energy trauma.
The patient shown in the X-ray had noticed swelling of the foot for approximately 3 weeks without any known injury. The X-ray shows several fractures (arrowheads) and a dislocation of the first metatarsal (arrow). Such a severe injury in patients without diabetes would be seen only after a high-energy trauma.