Arthritis refers to the inflammation of one or more joints, often leading to pain and stiffness. While it can affect any joint in the body, it is particularly common in the smaller joints of the foot and ankle, causing discomfort and limiting mobility.
With over 100 types of arthritis identified, many forms specifically impact the foot and ankle, making everyday activities like walking or enjoying hobbies more challenging.
Although arthritis has no definitive cure, various treatment options are available to manage its progression and alleviate symptoms. When treated effectively, individuals with arthritis can often control their pain, maintain an active lifestyle, and continue to enjoy a high quality of life
Anatomy of the Foot and Ankle: Understanding Their Role and Structure
The foot and ankle play a critical role in supporting the body during standing, walking, and running. They provide balance, absorb shock, and facilitate movement. The ankle joint consists of three primary bones that enable up-and-down motion, while the foot comprises 28 bones and over 30 joints, allowing a broad range of movements.
Many of these joints are protected by articular cartilage, a smooth, slippery tissue that ensures seamless movement by allowing bones to glide over one another. Surrounding the joints is the synovium, a thin membrane responsible for producing lubricating fluid that minimizes friction during movement.
Ligaments, which are tough bands of tissue, connect the bones and stabilize the joints. Meanwhile, muscles and tendons provide the strength and support needed for mobility.
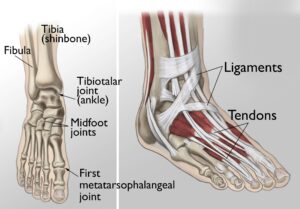 (Left) The joints of the ankle, midfoot, and big toe are commonly affected by arthritis. (Right) Ligaments connect the bones to each other, and tendons connect the bones to the surrounding muscles of the lower leg.
(Left) The joints of the ankle, midfoot, and big toe are commonly affected by arthritis. (Right) Ligaments connect the bones to each other, and tendons connect the bones to the surrounding muscles of the lower leg.
Common Types of Arthritis in the Foot and Ankle
Several types of arthritis commonly affect the foot and ankle, including osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis: The Wear-and-Tear Disease
Osteoarthritis, often referred to as degenerative arthritis, is prevalent among individuals as they age, though it can also affect younger people. This condition occurs when the cartilage within a joint gradually deteriorates. Over time, the cartilage becomes rough and frayed, reducing the protective space between bones. This can lead to bone-on-bone contact and the formation of painful bone spurs, known as osteophytes.
Risk factors for osteoarthritis include advancing age, obesity, and a family history of the condition. It develops slowly, typically causing increasing pain and stiffness over time.
Rheumatoid Arthritis: An Autoimmune Disorder
Rheumatoid arthritis is a chronic autoimmune disease that often begins in the foot and ankle, affecting multiple joints symmetrically across the body. This means the same joint on both sides of the body is typically involved.
In rheumatoid arthritis, the immune system mistakenly attacks the synovium, the protective lining of the joint. This leads to swelling and, over time, damage to cartilage, bone, ligaments, and tendons. Severe cases can result in joint deformity and disability.
While the exact cause remains unknown, genetic factors likely play a role, making some individuals more susceptible to the condition. A triggering event, such as an infection or environmental factor, often activates the immune system to attack the joints, leading to the onset of the disease.
 (Top) Osteoarthritis that has progressed to bone rubbing on bone and bone spurs. (Bottom) Swollen, inflamed synovium and joint deformity are signs of rheumatoid arthritis.
(Top) Osteoarthritis that has progressed to bone rubbing on bone and bone spurs. (Bottom) Swollen, inflamed synovium and joint deformity are signs of rheumatoid arthritis.
Anatomy of the Foot and Ankle: Understanding Their Role and Structure
The foot and ankle play a critical role in supporting the body during standing, walking, and running. They provide balance, absorb shock, and facilitate movement. The ankle joint consists of three primary bones that enable up-and-down motion, while the foot comprises 28 bones and over 30 joints, allowing a broad range of movements.
Many of these joints are protected by articular cartilage, a smooth, slippery tissue that ensures seamless movement by allowing bones to glide over one another. Surrounding the joints is the synovium, a thin membrane responsible for producing lubricating fluid that minimizes friction during movement.
Ligaments, which are tough bands of tissue, connect the bones and stabilize the joints. Meanwhile, muscles and tendons provide the strength and support needed for mobility.
Common Types of Arthritis in the Foot and Ankle
Several types of arthritis commonly affect the foot and ankle, including osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis: The Wear-and-Tear Disease
Osteoarthritis, often referred to as degenerative arthritis, is prevalent among individuals as they age, though it can also affect younger people. This condition occurs when the cartilage within a joint gradually deteriorates. Over time, the cartilage becomes rough and frayed, reducing the protective space between bones. This can lead to bone-on-bone contact and the formation of painful bone spurs, known as osteophytes.
Risk factors for osteoarthritis include advancing age, obesity, and a family history of the condition. It develops slowly, typically causing increasing pain and stiffness over time.
Rheumatoid Arthritis: An Autoimmune Disorder
Rheumatoid arthritis is a chronic autoimmune disease that often begins in the foot and ankle, affecting multiple joints symmetrically across the body. This means the same joint on both sides of the body is typically involved.
In rheumatoid arthritis, the immune system mistakenly attacks the synovium, the protective lining of the joint. This leads to swelling and, over time, damage to cartilage, bone, ligaments, and tendons. Severe cases can result in joint deformity and disability.
While the exact cause remains unknown, genetic factors likely play a role, making some individuals more susceptible to the condition. A triggering event, such as an infection or environmental factor, often activates the immune system to attack the joints, leading to the onset of the disease.
 This X-ray reveals osteoarthritis in the metatarsophalangeal joint of the big toe. Joint space narrowing (black arrow) and bone spurs (white arrows) can be seen.
This X-ray reveals osteoarthritis in the metatarsophalangeal joint of the big toe. Joint space narrowing (black arrow) and bone spurs (white arrows) can be seen.
Additional Diagnostic Tools for Arthritis in the Foot and Ankle
Advanced Imaging Techniques
In certain cases, specialized imaging tests such as bone scans, computerized tomography (CT) scans, or magnetic resonance imaging (MRI) scans are required to provide a clearer picture of the condition of bones and surrounding soft tissues. These advanced tests can help detect subtle abnormalities that may not appear on standard X-rays, ensuring a more precise diagnosis.
Laboratory Testing
To identify the specific type of arthritis, your doctor may recommend blood tests. These are particularly important for diagnosing inflammatory types of arthritis, such as rheumatoid arthritis. Blood tests can help detect markers associated with autoimmune diseases, providing essential information for an accurate diagnosis.
Referral to a Rheumatologist
If rheumatoid arthritis is suspected, your doctor may refer you to a rheumatologist. This specialist has expertise in diagnosing and managing autoimmune and inflammatory arthritis. While your symptoms and initial test results might indicate rheumatoid arthritis, a rheumatologist can confirm the diagnosis and consider other less common forms of inflammatory arthritis that might be contributing to your condition.
Treatment Options for Arthritis in the Foot and Ankle
While there is no cure for arthritis, a variety of treatments can help alleviate pain and improve mobility. Depending on the severity of your symptoms and the progression of the disease, your doctor may recommend nonsurgical or surgical interventions.
Nonsurgical Treatments
Lifestyle Modifications
Adopting certain changes in daily activities can relieve arthritis-related pain and slow the disease’s progression. These include:
- Reducing activities that exacerbate symptoms.
- Switching from high-impact exercises like jogging to low-impact activities such as swimming or cycling.
- Losing weight to reduce joint stress, resulting in less pain and improved function.
Physical Therapy
Targeted exercises can enhance flexibility, range of motion, and muscle strength in the foot and ankle. A customized program developed by your doctor or physical therapist can help alleviate symptoms. However, if therapy worsens joint pain by increasing friction, this treatment may be discontinued.
Assistive Devices
- Braces: Devices such as an ankle-foot orthosis (AFO) can enhance stability and mobility.
- Shoe Inserts and Orthotics: Custom orthotics or stiff-soled shoes with rocker bottoms can reduce joint pressure and pain. For deformities, specially designed inserts can realign the foot or ankle to minimize discomfort.
 A custom-molded leather brace can be effective in minimizing the pain and discomfort from ankle and hindfoot arthritis.
A custom-molded leather brace can be effective in minimizing the pain and discomfort from ankle and hindfoot arthritis.
Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen or naproxen can help reduce pain and swelling.
- Cortisone Injections: A steroid combined with an anesthetic, such as triamcinolone or methylprednisolone, can be injected into the joint to reduce inflammation and provide temporary pain relief.
Surgical Treatments
If nonsurgical methods fail to provide relief and arthritis significantly impairs your daily activities, surgery may be considered. The type of surgery depends on the location and severity of the arthritis.
Arthroscopic Debridement
This minimally invasive procedure is often effective in the early stages of arthritis. It involves removing loose cartilage, inflamed synovial tissue, and bone spurs from the affected joint to reduce pain and improve function.
 The surgeon holds the arthroscope in one hand and uses a thin instrument with their other hand to create another small incision.
The surgeon holds the arthroscope in one hand and uses a thin instrument with their other hand to create another small incision.
Surgical Techniques for Arthritis in the Foot and Ankle
Arthroscopic Surgery
Arthroscopy is a minimally invasive procedure where a surgeon inserts a small camera, called an arthroscope, into the foot or ankle joint. The camera projects images onto a monitor, allowing the surgeon to guide precise surgical instruments through small incisions, avoiding the larger cuts required for open surgery.
This technique is most effective when arthritis-related pain stems from bone spurs, and the joint space has not yet significantly narrowed due to cartilage loss. However, arthroscopy can sometimes accelerate joint deterioration. By removing bone spurs and increasing joint motion, the remaining cartilage may wear away more quickly.
Arthrodesis (Joint Fusion)
Arthrodesis involves fusing the bones of an arthritic joint to form a single, continuous bone. The procedure aims to alleviate pain by eliminating movement in the affected joint.
During the procedure, the surgeon removes the damaged cartilage and secures the bones in a fixed position using pins, plates, screws, or rods. Over time, the bones fuse together, much like how broken bones heal. Once the bones are permanently joined, joint pain is significantly reduced or eliminated since there is no longer any movement in the joint.
The surgeon holds the arthroscope in one hand and uses a thin instrument with their other hand to create another small incision.
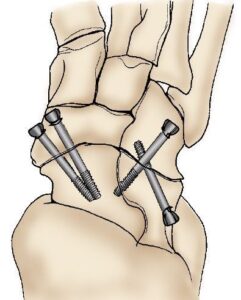 Screws are used to fuse the bones of the hindfoot and prevent painful motion.
Screws are used to fuse the bones of the hindfoot and prevent painful motion.
Success and Potential Complications of Arthrodesis
Arthrodesis, or joint fusion, is generally a highly effective procedure for relieving arthritis pain. However, like any surgery, it comes with potential risks and complications.
Nonunion (Incomplete Fusion)
In some cases, the bones may fail to fuse completely, a condition known as nonunion. This can result in persistent pain and swelling, even though the hardware used during the procedure, such as screws or plates, typically does not cause discomfort on its own. If nonunion occurs, additional surgery may be required to insert bone grafts or replace the hardware. However, subsequent fusion surgeries are less likely to succeed, making it essential to follow your doctor’s recovery recommendations diligently after the initial operation.
Wound Healing Issues
A small percentage of patients experience complications with wound healing. These issues are often manageable with proper local wound care, such as dressing changes. In rare cases, additional surgery may be necessary to address the problem.
Increased Stress on Surrounding Joints
After fusion, the loss of motion in the treated joint can place additional stress on adjacent joints. Over time, this increased strain may lead to arthritis in nearby joints, potentially causing pain and requiring further treatment years after the surgery.
Proper recovery practices and regular follow-ups with your doctor can help minimize these risks and ensure the long-term success of the procedure.
 (Left) X-rays show ankle arthritis. Joint spacing narrow (arrow) has resulted in bone rubbing on bone. (Right) A different arthritic ankle after treatment with arthrodesis. Screws are used to hold the bones in proper alignment until the fusion is complete.
(Left) X-rays show ankle arthritis. Joint spacing narrow (arrow) has resulted in bone rubbing on bone. (Right) A different arthritic ankle after treatment with arthrodesis. Screws are used to hold the bones in proper alignment until the fusion is complete.
Total Ankle Replacement (Arthroplasty): Restoring Joint Function
Total ankle replacement, or arthroplasty, is a surgical procedure where the damaged cartilage and bone in the ankle joint are removed and replaced with metal or plastic components. These artificial joint surfaces are designed to restore movement and improve overall joint function.
While total ankle replacement is less common than similar procedures for the hip or knee, advancements in implant technology have significantly improved outcomes. Modern designs make this option increasingly viable for individuals seeking to alleviate pain and regain mobility in the ankle joint.
 An X-ray of a total ankle replacement (arthroplasty).
An X-ray of a total ankle replacement (arthroplasty).
Total Ankle Replacement: Indications, Benefits, and Recovery
Who is a Candidate for Ankle Replacement?
Total ankle replacement is often recommended for individuals with:
- Advanced arthritis in the ankle.
- Severe joint damage caused by arthritis, leading to the destruction of joint surfaces.
- Persistent ankle pain that interferes with daily activities.
This procedure effectively relieves arthritis pain while preserving joint movement. Unlike fusion, which eliminates joint motion, ankle replacement allows for mobility, reducing stress on nearby joints and lowering the risk of developing adjacent joint arthritis.
Long-Term Considerations
As with any joint replacement, ankle implants may loosen or fail over time. In severe cases of implant failure, a revision surgery can replace the existing implant with a new one. Alternatively, the implant can be removed, and the joint fused. However, fusion after implant removal is more complex than initial fusion procedures. Bone grafts are required to fill gaps left by the removed implant, but these grafts may lack strength, increasing the risk of nonunion.
Recovery After Total Ankle Replacement
Pain Management
Foot and ankle surgery can be painful, but modern pain management techniques have made it easier to control discomfort. Immediately after surgery, pain relief medications will be administered. For home recovery, your doctor may prescribe short-term pain relievers to manage residual discomfort.
Post-Surgery Care
- A cast will likely be applied to immobilize the foot and ankle, preventing movement and reducing the risk of nonunion.
- Swelling can be minimized by elevating the foot above heart level for 1 to 2 weeks.
Physical Therapy and Mobility
As you recover, physical therapy may be recommended to strengthen the foot and ankle muscles and improve range of motion. Most patients can resume daily activities within 3 to 4 months, although full recovery may take 4 to 9 months depending on the initial severity of the condition and the complexity of the procedure. Supportive shoes or braces may be needed during this time to ensure proper healing.





