Introduction: Thumb osteoarthritis, particularly at the base of the thumb (the carpometacarpal or CMC joint), is a common and often debilitating condition. It leads to pain, reduced thumb mobility, and difficulty with everyday tasks like gripping or pinching. While many patients find relief with conservative treatments like physiotherapy, medications, or splinting, these methods are sometimes insufficient for severe cases. For those patients, total joint replacement can offer significant and long-lasting relief.
This article provides an in-depth look at total joint replacement for thumb osteoarthritis, its advantages, potential risks, and what to expect during recovery. It aims to give you a better understanding of this advanced surgical option and help you make informed decisions about your treatment.
What is Thumb CMC Joint Osteoarthritis?
The CMC joint at the base of the thumb is one of the most important joints for hand function, allowing a wide range of motion. Over time, wear and tear can cause the cartilage in this joint to deteriorate, leading to osteoarthritis. Symptoms include:
- Pain at the base of the thumb, especially during activities that involve gripping or pinching.
- Weakness and difficulty in performing tasks like opening jars or turning keys.
- Stiffness and limited range of motion.
- Visible changes in thumb shape or alignment.
Thumb CMC joint osteoarthritis is more common in women over the age of 50 but can affect both genders and younger individuals as well. It can significantly impact your quality of life, making even simple tasks painful.
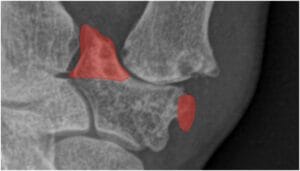
Removal of the medial and lateral osteophytes at the distal articular surface of the trapezium.
Why Consider Total Joint Replacement?
When conservative treatments (such as pain relievers, physiotherapy, and splints) fail to provide adequate relief, surgical options may be considered. While several surgical techniques are available, total joint replacement is gaining popularity for its ability to restore both function and appearance to the thumb. It offers several distinct advantages over traditional methods like trapeziectomy (removing part of the trapezium bone), which has been the standard treatment for many years.
Advantages of Total Joint Replacement:
- Faster Recovery:One of the most significant benefits of thumb joint replacement is a quicker recovery compared to other surgical options. Following surgery, immobilisation is either minimal or not required, allowing patients to resume normal activities much sooner. Studies show that patients who undergo total joint replacement typically experience faster functional recovery and shorter sick leave compared to those who have undergone trapeziectomy. In fact, most patients return to light activities within weeks rather than months.
- Restoration of Thumb Length and Alignment:
Osteoarthritis of the thumb CMC joint often leads to a shortening of the thumb and deformities, such as the “Z-deformity” where the thumb bends unnaturally due to joint instability. Total joint replacement corrects these deformities by restoring the natural length and alignment of the thumb. This not only improves the function of the hand but also provides a more aesthetically pleasing result. Patients are often much more satisfied with the appearance of their thumb after joint replacement compared to other procedures like trapeziectomy. - Reduced Risk of Complications in Adjacent Joints:
Unlike trapeziectomy, which involves removing part of the trapezium bone, total joint replacement preserves this structure. This preservation helps maintain stability in the surrounding carpal bones and reduces the risk of future arthritis or complications in adjacent joints. Keeping the trapezium intact also prevents further degeneration of the nearby scaphotrapeziotrapezoid (STT) joint, which is often a concern in patients who undergo more traditional surgeries. - No Need for Tendon Harvesting:
Traditional surgeries like trapeziectomy often require the use of a tendon from another part of the body to stabilise the thumb after bone removal. This can lead to additional complications, such as reduced strength in the donor area. In contrast, total joint replacement doesn’t require tendon harvesting, minimising the risks of such complications. - Higher Patient Satisfaction:
Data shows that patients who undergo total joint replacement tend to be more satisfied with their results compared to those who opt for trapeziectomy. This is due to a combination of faster recovery, better functional outcomes, and improved cosmetic results. According to studies, over 89% of patients who had thumb joint replacement would recommend the procedure, compared to 76% of trapeziectomy patients.
Surgical Procedure
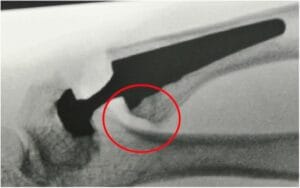
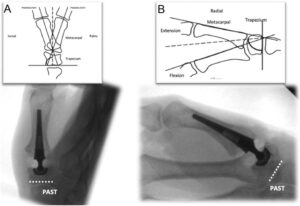
In total joint replacement for the thumb CMC joint, the damaged joint surfaces are removed and replaced with a prosthesis. The prosthesis typically consists of two parts: a metal stem that fits into the thumb’s metacarpal bone and a modular socket that sits in the trapezium bone. The metal-on-polyethylene design of the implant ensures smooth movement and reduces wear over time.
Steps of the Surgery:
- The surgeon makes a small incision near the base of the thumb to access the CMC joint.
- The damaged joint surfaces are carefully removed.
- The implant components (a stem and a cup) are positioned in the thumb and trapezium bones.
- The implant is secured, and the incision is closed.
Resection of the volar beak at the base of the thumb metacarpal.
The cup’s placement in the trapezium parallel with the proximal articular surface of the trapezium aligns it with the centre of motion of the normal thumb carpometacarpal joint.
The surgery is often performed under regional anaesthesia, allowing you to return home the same day.
Recovery and Rehabilitation
Initial Recovery: Recovery following total joint replacement is generally quicker than other surgical options. You will be encouraged to move your thumb gently soon after surgery to maintain mobility and prevent stiffness. A light splint may be used temporarily, but full immobilisation is not typically required.
Weeks 6-12: By this stage, you should notice significant improvements in pain and thumb function. You will gradually reduce your use of the splint and start strengthening exercises under the guidance of your physiotherapist. These exercises aim to restore strength and flexibility to the thumb, helping you return to your normal activities.
Long-Term Results: Most patients experience long-lasting pain relief and improved function after thumb joint replacement. Studies show a 10-year implant survival rate of over 90%, making it a reliable solution for thumb osteoarthritis. The majority of patients are able to resume their daily activities, including work and hobbies, with minimal discomfort.
Potential Risks and Complications
As with any surgery, there are risks associated with total joint replacement. These include:
- Implant loosening or dislocation: This can occur if the prosthesis shifts out of place. However, newer implant designs have significantly reduced the likelihood of this complication.
- Infection: As with any surgery, there is a small risk of infection, which can usually be treated with antibiotics.
- Fracture of the trapezium bone: This is rare but can occur if the bone is weakened during the procedure. Careful surgical technique reduces this risk.
Your surgeon will discuss these risks with you before surgery and take steps to minimise complications.
Is Total Joint Replacement Right for You?
Total joint replacement is an excellent option for patients with advanced thumb osteoarthritis who have not found relief with non-surgical treatments. It offers a faster recovery, better cosmetic results, and improved function compared to traditional surgeries like trapeziectomy. However, it is important to weigh the potential risks and benefits with your healthcare provider to determine if this surgery is the best option for you.
Exercises
Download the attached file From here
and make sure to stick to these exercises.