Introduction
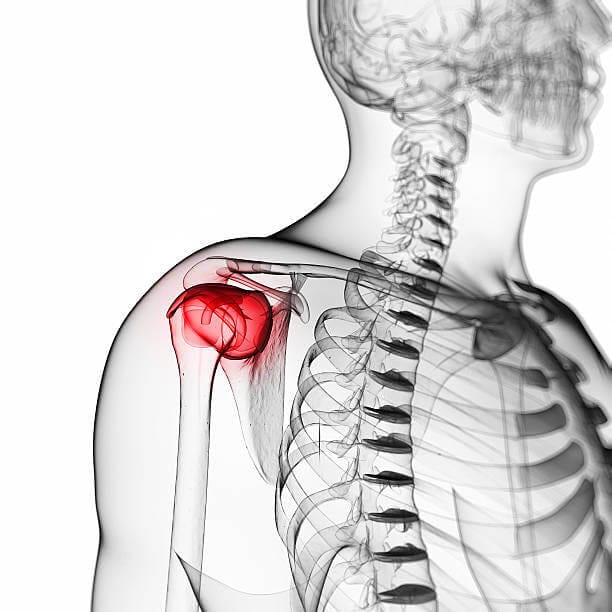
Bursitis is an inflammation of the bursa, a small fluid-filled sac that acts as a cushion between bones, tendons, joints, and muscles. In the arm, bursitis commonly affects the shoulder (subacromial bursitis) and elbow (olecranon bursitis). Recognizing and treating this condition is crucial for preventing chronic pain and disability, particularly in patients who are physically active or involved in repetitive motion tasks.
Pathophysiology
The bursa serves to reduce friction and allow smooth movement of the muscles and tendons over bones. Inflammation occurs when the bursa becomes irritated due to repetitive motion, direct trauma, or systemic conditions such as rheumatoid arthritis or gout. The inflamed bursa produces excess fluid, leading to swelling and pain, which can significantly impair joint function.
Clinical Presentation
Patients with bursitis in the arm typically present with localized pain, tenderness, and swelling over the affected bursa. In the case of subacromial bursitis, patients may experience pain with overhead activities or when lying on the affected shoulder. Olecranon bursitis often presents with noticeable swelling at the back of the elbow, which may be warm to the touch if infected (septic bursitis).
Diagnosis
Diagnosing bursitis requires a detailed history and physical examination. Imaging studies, such as ultrasound or MRI, can be useful in confirming the diagnosis and differentiating bursitis from other conditions like tendonitis, rotator cuff tears, or septic arthritis. Ultrasound can visualize the inflamed bursa and detect associated conditions such as cobblestoning in the fat layer overlying the bursa, which may suggest cellulitis.
In cases where infection is suspected, aspiration of the bursa fluid is essential. The aspirate should be sent for cell count, Gram stain, culture, glucose analysis, and crystal examination to rule out septic or crystal-induced bursitis.
Treatment
Conservative Management:
The cornerstone of bursitis treatment is conservative management, particularly in non-infectious cases. Rest, ice, compression, and elevation (RICE) are the first-line interventions. Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be prescribed to manage pain and inflammation. Patients should be educated on ergonomics and encouraged to avoid repetitive motions that exacerbate the condition.
Physical Therapy:
Physical therapy is crucial for maintaining joint mobility and preventing muscle atrophy, particularly in subacromial bursitis. Exercises should focus on strengthening the surrounding musculature to provide better support to the joint and reduce the recurrence of bursitis.
Corticosteroid Injections:
Corticosteroid injections can provide significant pain relief in cases of chronic or refractory bursitis. However, caution is advised, particularly with superficial bursae, as repeated injections can increase the risk of iatrogenic infections, tendon injury, or skin atrophy. In subacromialbursitis, corticosteroid injections may mask underlying conditions such as rotator cuff tears, delaying their diagnosis and treatment.
Surgical Intervention:
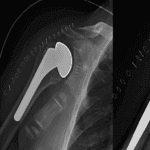
Surgery is rarely required but may be considered in cases of chronic bursitis unresponsive to conservative measures or if there is persistent infection. Surgical options include bursectomy, which can often be performed arthroscopically.
Infectious (Septic) Bursitis:
Management of septic bursitis involves antibiotic therapy tailored to the most likely pathogens, typically gram-positive bacteria such as Staphylococcus aureus. Empirical therapy should be guided by the results of fluid aspiration and sensitivity testing. In severe cases, hospitalization may be necessary for intravenous antibiotics and possible surgical drainage.
Differential Diagnosis
Bursitis can mimic or coexist with various other musculoskeletal conditions. For instance, subacromial bursitis may be confused with rotator cuff tears or shoulder impingement syndrome. Olecranon bursitis must be differentiated from conditions such as gout, rheumatoid arthritis, or elbow fractures. A thorough differential diagnosis is essential to ensure appropriate treatment and avoid complications.
Prognosis and Follow-Up
The prognosis for patients with bursitis is generally good, particularly with early and appropriate treatment. Most cases resolve with conservative management, though recurrence is possible if the underlying cause is not addressed. Regular follow-up is recommended to monitor the patient’s response to treatment and adjust the management plan as necessary.
Frequently Asked Questions
- How can I prevent bursitis from recurring?
- Preventing recurrence involves avoiding repetitive motion, improving ergonomics, and engaging in regular strengthening exercises to support the affected joint.
- Is it safe to continue physical activity with bursitis?
- Physical activity should be modified to avoid exacerbating the condition. Low-impact exercises that do not stress the affected bursa are recommended.
- When is surgery necessary for bursitis?
- Surgery is considered only in chronic cases unresponsive to conservative treatment or in cases of septic bursitis requiring drainage.
By adhering to these guidelines, healthcare providers can effectively recognize and treat bursitis, ensuring optimal outcomes for their patients.