Definition
An Essex-Lopresti injury, or longitudinal radioulnar dissociation (LRUD), occurs when a violent compressive load to the wrist results in a triad of injuries: disruption of the distal radioulnar joint (DRUJ), tear of the interosseous ligament complex (IOLC), and fracture of the radial head.
Anatomy
- Radial Head: The primary stabilizer of the radius, preventing proximal migration during axial wrist loads by its contact with the capitellum.
- Interosseous Ligament Complex (IOLC): The most critical secondary stabilizer of the forearm’s longitudinal axis, responsible for 71% of forearm stiffness after radial head resection.
- Triangular Fibrocartilage Complex: Contributes 8% to forearm longitudinal stiffness.
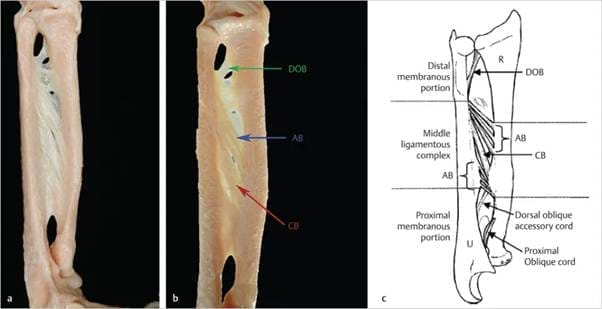
- IOLC Structure: Composed of five segments, with the central band being the stoutest and most crucial. The central band is 9.7 mm wide, 1-2 mm thick, and 40 mm long (FIG 1).
Pathogenesis
- Load Distribution: At the wrist, the radius transmits 80% of the axial load and the ulna 20%. The IOLC redistributes this load proximally so that at the elbow, the radiocapitellar joint bears 57% of the load, and the ulnohumeral articulation bears 43%.
- Injury Impact: In LRUD cases, a radial head prosthesis may restore axial stability but won’t address load distribution at the elbow if the IOLC doesn’t heal. This can lead to pain and early degenerative changes due to increased load on the radiocapitellar joint.
Natural History
- Undiagnosed Cases: The incidence of LRUD is likely underdiagnosed, with recent studies suggesting it may occur in 3% of radial head fractures.
- Progression: Without a competent radial head, axial forearm instability leads to progressive proximal radius migration, ulnocarpal abutment, and DRUJ dislocation.
- Delayed Treatment: Leads to unsuccessful outcomes in 80% of patients.
Patient History and Physical Findings
- History: Patients typically report a high-energy axial load on the forearm, such as a fall from height onto outstretched arms. Initial complaints often focus on the elbow, with possible forearm and wrist pain.
- Examination: All patients with a radial head fracture should be checked for DRUJ laxity and tenderness, forearm swelling, and tenderness along the interosseous space. Subacute presentations may involve ulnar-sided wrist pain following radial head excision or shortened fracture malunion.
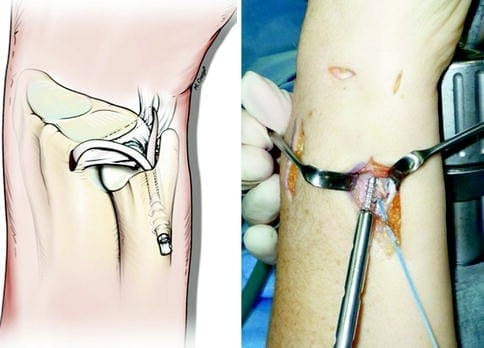
- Intraoperative Diagnosis: The radial pull test can help diagnose IOLC disruption. If the ulnar variance increases by 3 mm or more with 20 pounds of proximal radius traction, the IOLC is likely disrupted.
Imaging and Diagnostic Studies
- Radiographs: Standard radiographs of the affected elbow and forearm, and bilateral neutral forearm wrist posteroanterior (PA) views for comparing ulnar variance.
- MRI and Ultrasound: Effective in diagnosing IOLC injury with over 90% sensitivity and specificity. However, their clinical accuracy is debated.
- Bilateral Comparison: Maximum forearm interosseous space comparison in a cadaver LRUD model shows a 70% increase in space after IOLC disruption.
Differential Diagnosis
- Isolated radial head fracture
- Partial IOLC disruption
Nonoperative Management
- Mason Type 1 Fracture: Can be managed with a Muenster cast in a position where the DRUJ is reduced (usually maximum supination) for at least 8 weeks. However, structural integrity of the IOLC healing is uncertain.
Surgical Management
Acute Situations
- Repair or Replace Radial Head: Stabilize the DRUJ by splinting in supination or pinning the DRUJ.
Chronic Conditions
- Address Deficiencies:
- Radial head arthroplasty if possible.
- Ulnar shortening osteotomy.
- Central band reconstruction uses techniques such as pronator teres rerouting, autograft and allograft tendon, suture constructs, or bone-patellar tendon-bone graft.
Conclusion
Reconstruction for interosseous ligament disruption involves careful diagnosis, preoperative planning, and appropriate surgical techniques to address acute and chronic conditions. Proper management of LRUD can restore forearm stability and function, preventing long-term complications.